The UK Department of Health and Social Care’s aid-funded global health research and innovation
Score summary
The Department of Health and Social Care (DHSC) funds relevant and effective global health research and innovation portfolios and is working to enhance low- and middle-income country leadership of research projects, but increased attention to impact is needed.
A significant share of UK official development assistance (ODA) for health is spent on research, including through DHSC. Between 2018-19 and 2024-25, DHSC’s ODA spend on global health research will total almost £1 billion. This ODA is used to fund a Global Health Research portfolio of DHSC-managed partnerships and large programmes managed by the National Institute for Health and Care Research, and a Global Health Security research and innovation portfolio managed by DHSC. We find that both portfolios support research that is ODA-eligible and generally relevant to health challenges in low- and middle-income countries (LMICs). DHSC is working to improve LMIC access to research funding but has further to go in untying its aid and in embedding the principle of equitable partnership across all its research activities.
DHSC makes innovative use of community engagement and involvement to strengthen research projects and deliver localised benefits, and some projects are already contributing to improved health outcomes, most obviously through vaccine development for typhoid and COVID-19. LMIC researchers are also benefitting from support to develop their individual capacity. However, DHSC’s approach to capacity strengthening at the institutional and system levels is less considered, attention to research impact pathways is insufficient, and coordination in LMIC contexts with the Foreign, Commonwealth and Development Office is patchy. This limits the prospect of DHSC’s significant ODA expenditure contributing to transformational change and greater LMIC leadership in global health research.
Overall, DHSC’s ODA-funded global health research is focused on generating benefits for people in LMICs. ICAI observed a range of well-designed and context-appropriate projects, and some have already yielded impressive results. The department is taking a proactive approach to learning and is applying this on an ongoing basis to adapt its programming. We also see a positive trajectory on many of the challenges noted in our review.
| Individual question scores | |
|---|---|
| Relevance: How relevant are DHSC’s ODA-funded global health research portfolios to the UK’s strategic objectives on global health? |  |
| Effectiveness: How effectively does DHSC’s ODA-funded research contribute to improving global health outcomes? |  |
| Learning: Has the design of DHSC’s global health research portfolios been informed by its own monitoring, evaluation and learning, and by lessons from other ODA-funded health research? |  |
Acronyms and glossary
| Acronyms | |
|---|---|
| AARs | After Action Reviews |
| AMR | Antimicrobial resistance |
| CAB | Community advisory board |
| CAG | Community advisory group |
| CARB-X | Combating Antibiotic-Resistant Bacteria Biopharmaceutical Accelerator |
| CEI | Community engagement and involvement |
| CEPI | Coalition for Epidemic Preparedness Innovations |
| CHAI | Clinton Health Access Initiative |
| DFID | Department for International Development |
| DHSC | Department of Health and Social Care |
| DSIT | Department for Science, Innovation and Technology |
| ESSENCE | Enhancing Support for Strengthening the Effectiveness of National Capacity Efforts |
| FCDO | Foreign, Commonwealth and Development Office |
| FCDO EQuALS | Foreign, Commonwealth and Development Office, Evaluation Quality Assurance and Learning Service |
| FCDO RED | Foreign, Commonwealth and Development Office, Research and Evidence Directorate |
| FIND | Foundation for Innovative New Diagnostics |
| GAMRIF | The Global Antimicrobial Resistance Innovation Fund |
| GARDP | Global Antibiotic Research and Development Partnership |
| GCC | Grand Challenges Canada |
| GECO | Global Effort on COVID-19 Research |
| GHR | Global Health Research |
| GHS | Global Health Security |
| GRIPP | Getting research into policy and practice |
| HAC | Health advisory committee |
| HFF | Health Funders Forum |
| HIC | High-income country |
| IATI | International Aid Transparency Initiative |
| IDRC | International Development Research Centre |
| InnoVet AMR | Innovative Veterinary Solutions for Antimicrobial Resistance |
| ISAG | Independent Scientific Advisory Group |
| JGHT | Joint Global Health Trials Initiative |
| LGBTQIA+ | Lesbian, gay, bisexual, transgender, queer/questioning, intersex, asexual |
| LMICs | Low- and middle-income countries |
| MEL | Monitoring, evaluation and learning |
| MERS | Middle East Respiratory Syndrome |
| MLW | Malawi Liverpool Wellcome |
| MODARI | Mapping ODA research and innovation |
| MRC | Medical Research Council |
| NIHR | National Institute for Health and Care Research |
| NIHR Global HPSR | National Institute for Health and Care Research, Global Health Policy and Systems Research |
| NIHR RIGHT | National Institute for Health and Care Research, Research and Innovation for Global Health Transformation |
| ODA | Official development assistance |
| OECD-DAC | Development Assistance Committee of the Organisation for Economic Cooperation and Development |
| R&D | Research and development |
| RSTMH | Royal Society of Tropical Medicine and Hygiene |
| SCOR | Strategic Coherence for ODA-funded Research |
| SDGs | Sustainable Development Goals |
| SIN | Science and Innovation Network |
| SPARC | Short Placement Award for Research Collaboration |
| SR | Spending Review |
| TDR | The Special Programme for Research and Training in Tropical Diseases |
| UK-PHRST | UK Public Health Rapid Support Team |
| UKCDR | UK Collaborative on Development Research |
| UKRI | UK Research and Innovation |
| UKVN | UK Vaccine Network |
| WHO | World Health Organisation |
| Glossary of key terms | |
|---|---|
| Aid untying | The practice of removing restrictions that require aid to be spent on goods and services from the donor country or from a small group of specified countries. Untied aid can be used to purchase goods and services from any country, promoting greater efficiency and effectiveness in aid delivery, and improving value for money. |
| Antimicrobial resistance (AMR) | The ability of microorganisms, such as bacteria, viruses, parasites and fungi, to resist the effects of antimicrobial drugs, rendering them ineffective in treating infections. |
| Capacity building | The planned development or increase in knowledge, output rate, management, skills, and other capabilities of an organisation through acquisition, incentives, technology and training. It is a process that supports the initial stages of building or creating capacities, assuming that there are no existing capacities to start from. |
| Capacity strengthening | The process of developing and enhancing the capabilities of individuals, organisations and systems to perform functions, solve problems, and set and achieve objectives in a sustainable manner. In global health research, the focus is on strengthening capacity to conduct, manage, share and apply research in ways that inform health policy and practice. |
| Equitable research partnerships | Collaborations between researchers and institutions that are based on mutual respect, shared responsibilities and shared benefits. These partnerships aim to ensure fair distribution of resources, recognition and opportunities, especially between high-income and low- and middle-income countries. |
| Global disease burden | The collective impact of diseases, injuries and risk factors on the health of populations worldwide, often measured in terms of mortality, morbidity, disability-adjusted life years, or economic costs. |
| Global health | A field of study, research and practice that prioritises improving health and achieving equity in health for all people worldwide. It addresses transnational health issues, determinants and solutions, involving many disciplines within and beyond the health sciences. |
| Global health research | International scientific study aimed at understanding health issues, developing interventions, and improving health outcomes across diverse populations and regions. |
| Health systems | The organisations, people and actions whose primary purpose is to promote, restore, or maintain health. This includes the provision of health services, a well-performing workforce, health information systems, access to essential medicines, financing, leadership and governance. |
| Infectious disease | A disease caused by pathogenic microorganisms, such as bacteria, viruses, parasites, or fungi, which can spread directly or indirectly from one person to another. |
| Innovation | The process of translating an idea or invention into a good or service that creates value or for which customers will pay. In the context of global health, it involves developing new methods, products, or services that improve health outcomes. |
| Noncommunicable diseases (NCDs) | Chronic diseases that are not passed from person to person. They include cardiovascular diseases, cancers, chronic respiratory diseases and diabetes. NCDs are often caused by genetic, physiological, environmental and behavioural factors. |
| Pandemic | An epidemic that has spread over multiple countries or continents, affecting a large proportion of the global population and requiring coordinated international efforts to control and mitigate its impact. |
| Pathogen | A microorganism, such as a virus, bacterium, parasite, or fungus, that can cause disease in its host. |
| R&D (Research and development) | The process of scientific investigation, experimentation and innovation aimed at discovering new knowledge, technologies, products, or solutions to address various challenges and needs. |
| Social and environmental determinants of health | The non-medical factors and conditions relating to society and the environment, including economic and cultural characteristics, that influence an individual’s health status and well-being. These determinants encompass aspects such as income, education, employment, housing, access to healthcare, social support networks, environmental quality and exposure to hazards. Understanding and addressing these factors is essential for promoting health equity and improving overall population health outcomes. |
Executive summary
Global health research aims to advance knowledge and innovation to improve health outcomes and achieve health equity globally, with particular attention to health challenges and potential solutions in low- and middle-income countries (LMICs). In recent decades, the UK has played an important role in many global health research initiatives and programmes, contributing funds from the official development assistance (ODA) budget managed by the former Department for International Development (DFID). The 2015 Aid Strategy broadened this responsibility, and the Department of Health and Social Care (DHSC) received its first ODA allocations, including for global health research, through the 2015 spending review. In 2023, DHSC’s ODA spend was the third-largest of all government departments, after the Foreign, Commonwealth and Development Office (FCDO) and the Home Office.
DHSC’s ODA for global health research is now considerable and will total almost £1 billion over the period 2018-19 to 2024-25. This funds two portfolios. The first, Global Health Research (GHR), consists of programmes managed through the National Institute for Health and Care Research (NIHR) and partnerships managed by DHSC. The second portfolio, Global Health Security (GHS) research and innovation, is managed by DHSC as part of wider departmental and UK government efforts to improve health security and health resilience.
The purpose of this review is to assess the relevance of DHSC’s strategy and approach to global health research and the effectiveness of its programming in this area. It also looks at how well the department is learning and adapting its global health research portfolios.
Relevance: How relevant are DHSC’s ODA-funded global health research portfolios to the UK’s strategic objectives on global health?
DHSC’s programming aligns with UK government strategies related to global health research, which prioritise economic and trade objectives alongside resilience to health threats. In developing its ODA-funded research portfolios, DHSC initially aimed to complement the work of other government departments, funding research in the areas of global health security, non-communicable diseases and health issues affecting people in ODA-eligible middle-income countries (rather than low-income countries). However, DHSC’s focus has broadened considerably over time, to include research areas where FCDO has been active such as health systems, to address health challenges in low-income countries, and to fill funding gaps. In interviews with ICAI, several stakeholders commented on the increased breadth of DHSC and NIHR programming, perceiving a lack of focus or comparative advantage. Some stakeholders also raised the question of whether NIHR’s initial narrow remit had made it more difficult to spend its ODA allocation.
ICAI’s country case studies and citizen engagement confirmed that the research projects funded by DHSC are generally relevant to the health challenges experienced in LMICs, including issues that are stigmatised or underfunded. Projects seek to identify and test appropriate solutions to these challenges, in some cases through multi-country clinical trials.
ICAI found that DHSC takes account of global stakeholder and expert views when scoping new areas of programming, including through an Independent Scientific Advisory Group that influences the shape of the GHR portfolio and has strong LMIC expert participation. This portfolio is also informed by DHSC involvement in fora that bring together UK and international funders of health and development research. However, DHSC has no staff in-country, or processes for engaging with the research priorities of LMIC governments, and aside from in India, we found from interviews and our three country case studies that the department has little engagement with UK embassies and FCDO health advisers. This limits opportunities for DHSC to connect its ODA-funded portfolios with national health research plans, FCDO programming, or the work of other development partners in LMICs.
DHSC references ‘equitable partnerships’ as a principle guiding the development and implementation of its ODA-funded research. NIHR provides its applicants with guidance to support the development of equitable partnerships between UK and LMIC researchers, and additional funds have been made available through some programmes to enable LMIC researchers to participate in the design of research projects and the ultimate dissemination of findings. Nevertheless, until recently, most of DHSC’s global health research programmes required projects to be led by UK institutions. While the majority of schemes are now opening calls to LMIC proposals, few applicants have been successful, even for projects that need no science and innovation infrastructure. This lack of success indicates a need for process adjustments or improved guidance and support for LMIC applicants, as well as for wider capacity strengthening. Furthermore, LMIC researcher voices are missing from many learning activities and in project and programme reporting, and feedback loops from LMIC communities and stakeholders to DHSC are limited, even where community engagement and involvement approaches are used at project level.
DHSC told ICAI that it is committed to the principle of aid untying. However, its approach to doing so in global health research seems inconsistent. In interviews with DHSC and NIHR, when asked about aid untying, responses almost always conflated this with the different but linked objectives of equitable partnership with and direct funding to institutions in LMICs. Among DHSC’s programmes, the Global Antimicrobial Resistance Innovation Fund offers the best example of aid untying, where delivery partners are selected with the aim of funding the best science to meet global health needs and leverage additional investment, with few if any geographical restrictions. However, until late 2020, NIHR was unable to issue contracts to non-UK entities, and NIHR appears comfortable with UK institutions being the only high-income country participants engaged through its programming. This has limited the ability of LMIC institutions to choose their research partners, going against the general stance of the Development Assistance Committee of the Organisation for Economic Cooperation and Development (OECD-DAC), the body overseeing aid rules, that untying fosters aid effectiveness.
DHSC programming is generally well aligned with the DAC’s ODA eligibility criterion related to LMIC primary benefit, and NIHR has established robust processes for screening proposals for ODA eligibility and for managing ODA funds. However, NIHR’s financial reporting is used to monitor ongoing ODA eligibility and the requirements are burdensome, particularly for LMIC researchers.
We award DHSC a green-amber score for relevance, in recognition of the department’s efforts to complement other funders of global health research and to address topics that are underfunded relative to the illness, injury and death they cause. DHSC is attentive to the issue of ODA eligibility, and the department is working to improve LMIC access to its funding schemes, but it has further to go in ensuring that its research partnerships are equitable and to untie aid.
Effectiveness: How effectively does DHSC’s ODA-funded research contribute to improving global health outcomes?
DHSC-funded global health research projects offer the prospect of improving health practice and ultimately health outcomes. ICAI visited projects in India and Malawi that were testing healthcare interventions or developing new products with the potential to improve outcomes in neonatal and maternal health or communicable diseases, for example. Some DHSC-funded projects are already contributing to improved health outcomes, most obviously through the development of vaccines, such as for typhoid and COVID-19. However, project-level monitoring primarily captures research activities and outputs, as well as some localised benefits delivered through community engagement and involvement (CEI) approaches, in areas such as health promotion and patient advocacy. More generally, NIHR’s CEI requirements have encouraged researchers to engage communities in their projects, with community advisory groups in Malawi involved in the design and delivery of research activities, patient recruitment and community outreach.
Many programmes lack detailed results frameworks, and approaches to impact reporting vary. For example, the GHR portfolio uses theories of change alongside a core indicator set against which all programmes should report, although some indicators are optional, and reporting is not consistent. The GHS programmes use logical frameworks (logframes) with targets and milestones, but unrealistic output and outcome targets mean some of these have not been very useful. In addition, many programmes indicate a patchy understanding of pathways for evidence translation, which could limit their potential to shape policy and practice. In part, this reflects limited guidance from DHSC and NIHR, including on more complex pathways to impact involving rigorous evidence synthesis. Collaboration between DHSC and FCDO has enabled some projects to access additional funding and partnerships to advance their research or bring new products to market. However, such potential is constrained by DHSC’s patchy engagement with FCDO health and science advisory networks, which also lack capacity, and by the lack of up-to-date and easily accessible data about many of the research projects funded by DHSC ODA.
DHSC and NIHR have stated an intent to strengthen LMIC research capacity at individual, institutional and system levels, consistent with UK and international definitions and guidance. In practice, DHSC capacity-strengthening initiatives focus on individuals, with demonstrable impact at this level. Almost 1,000 individuals who have been funded or otherwise supported through DHSC’s GHR portfolio have received advice and support as members of the NIHR GHR Academy (which offers training and development opportunities). Around 90% of NIHR GHR Academy members are from LMICs, and many researchers have been funded to complete postgraduate degrees. Some DHSC programmes have provided training in technical skills, in areas such as clinical trials and vaccine manufacture. ICAI found that this support is welcomed, particularly by early- and mid-career researchers in LMICs. However, without associated growth in institutional and system-level capacity, there is a clear risk of individual capacity ebbing away through researchers moving out of the sector or relocating. Some DHSC programmes do include complementary support to institutional capacity strengthening, for example in financial management, and ICAI visited laboratories in India that had been upgraded under one project. However, institutional capacity-strengthening outcomes are not systematically monitored and only one relatively recent programme (which was not in our sample) has a focus on this. DHSC ambitions related to system-level capacity strengthening are also unclear, and the department’s ODA funds are spread widely and thinly, limiting their transformative potential.
We have awarded DHSC’s global health research programming a green-amber score for effectiveness. This reflects some impressive achievements in areas such as vaccine development, alongside the department’s innovative use of CEI to strengthen research projects and deliver localised benefits, and its evident contribution to strengthening individual research capacity in LMICs. However, DHSC is not sufficiently deliberate in planning, monitoring and reporting its contribution to strengthening institutional and system-level capacity. The department is not doing enough to realise the transformative potential of its large GHR portfolio through, for instance, promoting rigorous evidence synthesis, or by supporting the uptake of research findings and innovations through purposeful collaboration with FCDO.
Learning: Has the design of DHSC’s global health research portfolios been informed by its own monitoring, evaluation and learning, and by lessons from other ODA-funded health research?
DHSC is an active participant in fora that enable the department to learn from other UK and international funders of global health research. When DHSC was first allocated ODA, the department engaged proactively with DFID to understand how to spend this money effectively. Since then, learning and coordination have become more ad hoc and dependent on personal relationships. NIHR’s ODA learning curve appears to have been steeper than necessary due to an emphasis on learning by doing, rather than learning from and adapting relevant elements of established ODA approaches used by the Medical Research Council, Wellcome and DFID/ FCDO, such as the effective use of logframes for research projects or best practice in developing pathways to research impact. NIHR has, however, since sought help from FCDO in specific areas.
There has been limited portfolio-level learning within DHSC, particularly related to impact, until recently. However, within the GHR portfolio, this is starting to improve, aided by NIHR’s engagement of a new GHR programme director and a recently concluded GHR portfolio evaluation. Reviews are also planned of the portfolio-level theory of change and of key areas such as CEI. However, while learning is evident within GHS programmes, there is currently no formal approach for GHS portfolio-level learning. There are also few mechanisms within DHSC for cross-portfolio learning between GHR and GHS on shared principles and challenges, such as equitable partnerships and capacity strengthening.
Formal monitoring and evaluation mechanisms are not yet used consistently across the GHR and GHS portfolios, and DHSC has been slow to complete and publish programme-level annual reviews. However, ICAI found good evidence that, where evaluations have been conducted, findings are being used to support learning and improvement. For example, all GHS programmes have been evaluated, with the recommendations shaping future programme phases.
Mechanisms for learning and adaptation within programmes have improved during the period under review. Some programmes have been specifically designed to pilot new approaches and to enable iterative learning and adaptation, in particular the Research and Innovation for Global Health Transformation programme. After Action Reviews are also well used by DHSC and NIHR to support learning and improvement within and across programmes. Although these and many other learning activities have been UK-dominated, there are some signs that LMIC researchers are becoming more involved, including through country-level roundtables convened by DHSC and NIHR.
With an increased emphasis on learning and adaptation evident, alongside some signs of improved engagement by LMIC researchers, DHSC is strengthening its ability to share, scale up and adapt effective global health research practice across its GHR portfolio, if not yet across the GHS portfolio. The department is evidently keen to adapt and improve its ODA-funded programming, and it has used opportunities to pilot and innovate to good effect. In recognition of this, we award a green-amber score for learning.
Recommendations
Recommendation 1: DHSC should focus on pathways to impact across its global health research portfolios, including by strengthening guidance for potential applicants and putting in place mechanisms for planning and measuring impact.
Recommendation 2: DHSC should ensure that its principle of equitable partnership is embedded and tracked across all areas of activity related to its global health research portfolios, including research funding, knowledge translation, learning, programme monitoring and evaluation.
Recommendation 3: DHSC should progressively untie its aid for global health research, to ensure value for money and to allow low- and middle-income country researchers to identify the most appropriate partners for their projects.
Recommendation 4: DHSC should purposively collaborate with FCDO to strengthen UK health ODA coherence and alignment to partner country needs and priorities.
Recommendation 5: DHSC and NIHR should take a more strategic approach towards institutional and system-level capacity strengthening in low- and middle-income countries, and develop metrics to track plausible contributions in these areas.
1. Introduction
1.1 Global health research aims to advance knowledge and innovation to improve health outcomes and achieve health equity globally. As the burden of ill health is highest in low- and middle-income countries (LMICs), studies are centred on problems and solutions in these contexts. This area of research grew significantly in scale and importance globally during the COVID-19 pandemic, and it has become more central to the strategic priorities of the UK international development programme. Aid-funded global health research is also central to the UK’s contribution to achieving the Sustainable Development Goals (SDGs) (see Box 1).
2.2 This is the first ICAI review that looks at global health research as a topic and the first to focus solely on aid spending by the UK Department of Health and Social Care (DHSC), which until now has not been covered as extensively as other government departments that spend large amounts of official development assistance (ODA). The review adds value by casting a light on an area of aid expenditure that has received little attention from scrutiny bodies. Our review questions are set out in Table 1.
1.3 The review looks at currently active and recently closed DHSC ODA-funded global health research and innovation programmes, particularly those that have been active since 2018. It covers programmes that aim to advance knowledge as a global public good, as well as to generate research and innovation with intended benefits for LMICs. These programmes fall into two broad portfolios: a Global Health Research (GHR) portfolio, with some of the research managed through the National Institute for Health and Care Research (NIHR) and the rest through partnerships managed by DHSC, and a Global Health Security (GHS) research and innovation portfolio managed by DHSC.
1.4 Programming that is out of scope for this review includes research funding calls that are still in the commissioning phase, and global health security programmes that are not focused on research and innovation such as the Fleming Fund. The deployment and capacity-building components of the UK Public Health Rapid Support Team were also deemed out of scope. We reviewed a sample of the programmes that were in scope. The full list of sampled programmes can be found in Annex 1.
1.5 This review builds on earlier ICAI reviews, including the review of the UK’s response to global health threats and research-focused reviews such as those of the Global Challenges Research Fund and the Newton Fund. It is also linked to ICAI’s COVID-19 reviews. ICAI’s synthesis review of findings from ICAI reports between 2019 and 2023 specifically mentions global health research, and it notes that DHSC awards to Oxford University through the UK Vaccine Network from 2016 onwards laid important foundations for, and subsequently supported, the development of the Oxford-AstraZeneca COVID-19 vaccine.
Box 1: Global health research and the Sustainable Development Goals
The UN Sustainable Development Goals, also known as the Global Goals, are a universal call to action to end poverty, protect the planet and ensure all people enjoy prosperity and peace. Funding for global health research directly supports Goal 3 on good health and well-being and Goal 9 on fostering innovation, which contributes to Goal 8 on decent work and economic growth. Goal 17 echoes the need for equitable partnerships between low- and middle-income countries and high-income countries to conduct global health research.
![]() Goal 3: Ensure healthy lives and promote well-being for all at all ages. The targets and indicators for this goal include vaccine coverage, access to medicines, and total ODA to medical research and basic health sectors.
Goal 3: Ensure healthy lives and promote well-being for all at all ages. The targets and indicators for this goal include vaccine coverage, access to medicines, and total ODA to medical research and basic health sectors.
Goal 8: Promote sustained, inclusive and sustainable economic growth, full and productive employment and decent work for all. Targets for this goal underline the importance of innovation to economic development.
8: Promote sustained, inclusive and sustainable economic growth, full and productive employment and decent work for all. Targets for this goal underline the importance of innovation to economic development.
 Goal 9: Build resilient infrastructure, promote inclusive and sustainable industrialisation and foster innovation. The targets and indicators for this goal include numbers of researchers as well as research and development expenditure as a share of gross domestic product.
Goal 9: Build resilient infrastructure, promote inclusive and sustainable industrialisation and foster innovation. The targets and indicators for this goal include numbers of researchers as well as research and development expenditure as a share of gross domestic product.
![]() Goal 17: Strengthen the means of implementation and revitalise the Global Partnership for Sustainable Development. This goal includes targets and indicators related to capacity building, to enhancing knowledge sharing and access to science, technology and innovation, and to North-South, South-South and triangular cooperation.
Goal 17: Strengthen the means of implementation and revitalise the Global Partnership for Sustainable Development. This goal includes targets and indicators related to capacity building, to enhancing knowledge sharing and access to science, technology and innovation, and to North-South, South-South and triangular cooperation.
Table 1: Our review questions
| Review criteria and questions | Sub-questions |
|---|---|
| Relevance: How relevant is DHSC’s ODA-funded global health research portfolio to the UK’s strategic objectives on global health? | •Does DHSC have a credible strategy for directing health research to meet global health needs and priorities? •How appropriate is DHSC’s approach to building equitable research partnerships? •How effectively does DHSC screen and monitor its research grants for ODA eligibility and for consistency with UK commitments on tied aid? |
| Effectiveness: How effectively does DHSC’s ODA-funded research contribute to improving global health outcomes? | •How well has DHSC-funded global health research contributed to improvements in health practice in low- and middle-income countries? •How well have DHSC-funded research programmes disseminated their results and supported other pathways to impact? •How well has DHSC enhanced research capacity in low- and middle-income countries? |
| Learning: Has the design of DHSC’s research portfolio been informed by its own monitoring, evaluation and learning, and by lessons from other ODA-funded health research? | •How well has DHSC learned from other ODA programmes that aim to carry out research or to build research and innovation capacity? • How well do DHSC managers of global health research programmes and their implementers adapt in response to lessons learned? |
2. Methodology
2.1 The methodology for this review has been designed around five components (Figure 1).
Figure 1: Review methodology
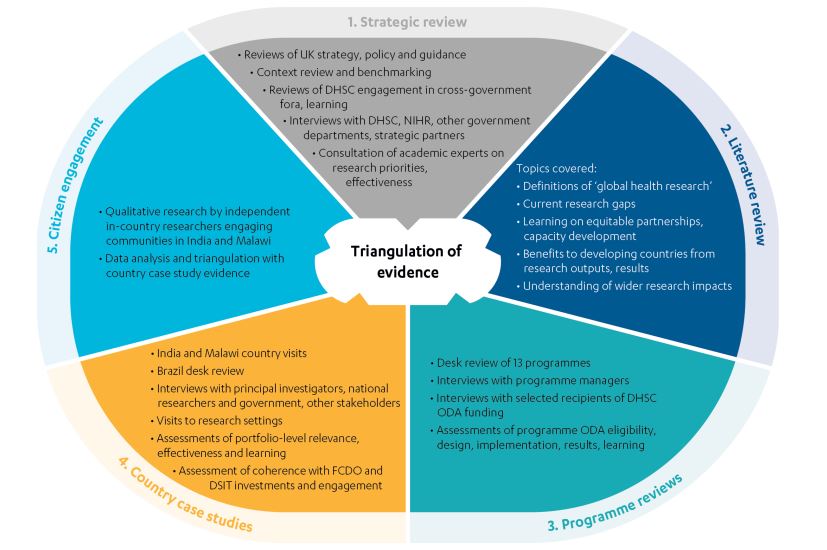
2.2 As set out in Figure 1, the components of our methodology enabled us to address our review questions and ensure sufficient triangulation of findings:
- Strategic review: The strategic review covered relevant UK government and Department of Health and Social Care (DHSC) strategies, policies and guidance related to global health research, alongside guidance on official development assistance (ODA) and research from the World Health Organisation (WHO) and the Organisation for Economic Cooperation and Development’s Development Assistance Committee (OECD-DAC), which the UK is expected to follow. It also examined DHSC engagement in coordination and learning mechanisms. Document review was complemented by interviews with a wide range of UK government representatives, DHSC delivery partners and external stakeholders.
- Literature review: The literature review covered relevant peer-reviewed literature on global health research alongside key grey literature, enabling us to assess DHSC’s approach in relation to the broader evidence base.
- Programme reviews: We conducted desk reviews of 13 DHSC programmes (see Table 2) identified using the sampling criteria outlined in our approach paper. We examined relevant documents and conducted interviews with programme managers in DHSC, the National Institute for Health and Care Research (NIHR) and relevant partner organisations, as well as with selected research institutions. The programme reviews focused on whether programme designs are evidence-based and consistent with rules on ODA eligibility and commitments to untied aid, whether programmes are implemented effectively and achieving their intended results, and the degree to which learning leads to adaptation and improvement.
- Country case studies: We conducted two country visits to India and Malawi and one country desk review of Brazil. The case studies assessed the DHSC global health research portfolio in each country (Figure 2), collecting and analysing evidence from interviews with principal investigators and other researchers, national government, FCDO staff in LMICs, and other stakeholders (Figure 3). Information from the country visits was triangulated with project and programme documentation, as well as with feedback from citizen engagement research in India and Malawi.
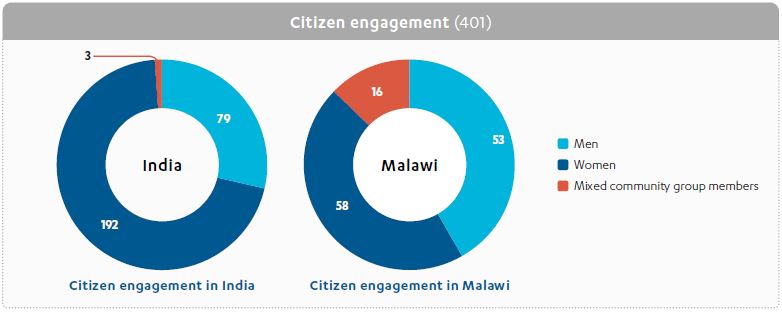
- Citizen engagement (with people affected by or expected to benefit from UK aid): ICAI is committed to incorporating the voices of people affected by UK aid into its reviews. Qualitative research in India and Malawi was undertaken by national research partners. Their consultations included citizens in poorer communities who are expected to benefit from research outputs such as new health products or technologies, and a small number of community groups advising DHSC ODA-funded research projects and institutions (see Figure 3).
Table 2: Programme sample
| Programmes | Spend (actual and projected) in review period | Brief description |
|---|---|---|
| NIHR-managed programmes | ||
| NIHR Global Health Research Groups | £145.93m | The NIHR Global Health Research Groups programme funds research to address locally identified challenges in LMICs, by supporting equitable research partnerships between researchers and institutions in LMICs and the UK. It aims to generate evidence for improved health outcomes and build sustainable research capacity in LMICs. Funding is available to research groups either new to delivering applied health research globally or wishing to expand an existing partnership. |
| NIHR Global Health Research Units | £103.63m | The NIHR Global Health Research Units programme funds ambitious collaborative research projects to address locally identified challenges in LMICs, by supporting equitable partnerships between universities and research institutes in LMICs and the UK. It aims to generate evidence for improved health outcomes and strengthen research capabilities in LMICs. Funding is awarded to partnerships with established track records in delivering internationally recognised global health research. |
| NIHR Research and Innovation for Global Health Transformation (RIGHT) | £73.09m | The NIHR RIGHT programme funds interdisciplinary applied health research in LMICs on areas of unmet need where a strategic and targeted injection of funds can result in a transformative impact. It prioritises research benefitting LMIC populations while fostering capacity building and knowledge exchange through equitable partnerships in LMICs and between LMIC and UK researchers, and by promoting interdisciplinary collaboration. Each funding opportunity has a focus on a different thematic priority. |
| NIHR Global Health Policy and Systems Research (Global HPSR) | £32.09m | The NIHR Global HPSR programme funds health policy and systems research that is directly and primarily of benefit to people in LMICs, by supporting equitable partnerships in LMICs and between LMICs and the UK. It aims to generate evidence to improve health systems and inform policy and practice in LMICs, which will lead to improved outcomes for the most vulnerable and address issues of health equity. |
| NIHR Global Research Professorships | £18.65m | The NIHR Global Research Professorships programme funds research leaders with a track record of applied health research in LMICs, to promote effective translation of research and to strengthen research leadership at the highest academic levels. |
| NIHR partnership programmes | ||
| NIHR-Wellcome Global Health Research Partnership – Wellcome | £16.96m | The NIHR-Wellcome Global Health Research Partnership funded existing work developed by Wellcome to support postgraduate students and postdoctoral and early-career researchers from LMICs and the UK, with a focus on research in health priority areas for LMICs and activities to improve research uptake into policy. |
| Global Effort on COVID-19 (GECO) Health Research – MRC | £8.07m | GECO was a rapid UK cross-government funding call aiming to support applied health research that would address COVID-19 knowledge gaps in ODA-eligible countries, aligned to the WHO COVID-19 research roadmap. |
| Joint Global Health Trials Initiative (JGHT) – MRC | £30.40m | JGHT is a UK cross-government initiative aiming to generate new knowledge to contribute to improving health in LMICs. It focuses on late-stage clinical research and smaller pilot studies that yield implementable results and address the major causes of mortality or morbidity in LMICs. |
| Royal Society of Tropical Medicine and Hygiene (RSTMH) Small Grants/Early Career Grants Scheme – RSTMH | £4.94m | The RSTMH Early Career Grants Scheme supports LMIC-based early-career researchers to develop their research skills and expertise. This partnership contributes to the NIHR Global Health Research priority to strengthen research capacity in LMICs. |
| Global Mental Health programme – Grand Challenges Canada (GCC) | £6m | This programme supports high-impact innovations that improve treatments and expand access to care for people living with or at risk of mental health disorders, with a focus on the mental health needs of young people in LMICs. |
| Global health security research and innovation programmes | ||
| UK Public Health Rapid Support Team (UK-PHRST) – research component | £13.90m | The research component of UK-PHRST collaborates with partners to conduct research to develop the evidence base for best practice in epidemic preparedness and response in ODA-eligible countries, and to develop local research capacity. |
| Global Antimicrobial Resistance Innovation Fund (GAMRIF) | £114.14m | GAMRIF is a UK aid fund that supports research and development around the world to reduce the threat of antimicrobial resistance in humans, animals and the environment, for the benefit of people in LMICs. |
| UK Vaccine Network (UKVN) | £137.08m | UKVN targets funds to support the development of new vaccines and vaccine technologies for emerging infectious disease threats in LMICs, to support better control in the future of disease outbreaks that risk becoming epidemics. |
2.3 A more detailed table with key data for each sampled programme is in Annex 1.
2.4 Figure 2 demonstrates how our programme sample was reflected in the country case studies for this review, and it shows the number of relevant project teams that were interviewed in each country context.
Figure 2: Sampling infographic
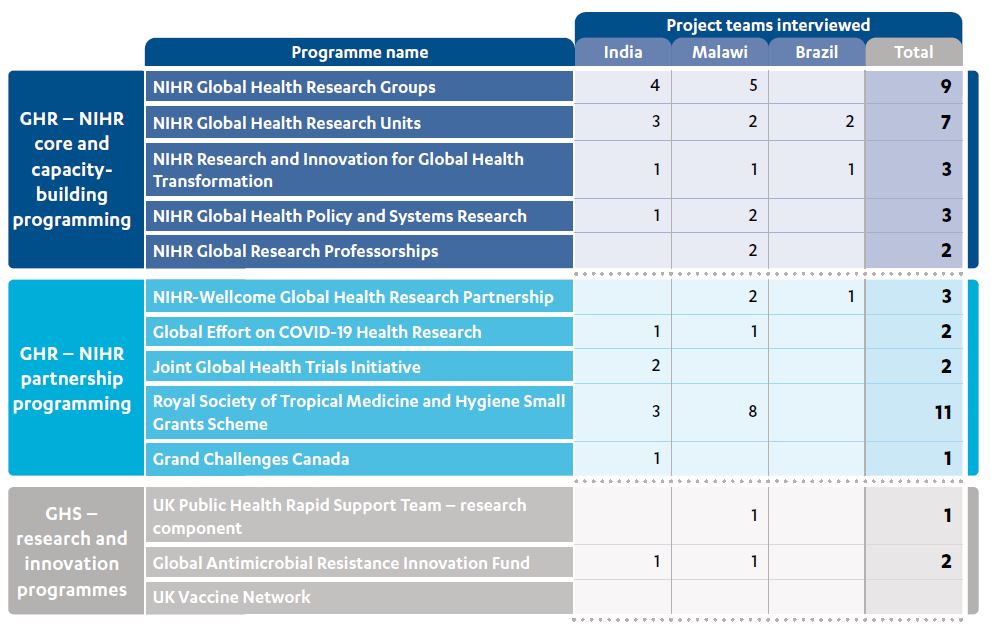
Figure 3: Sample of stakeholders consulted
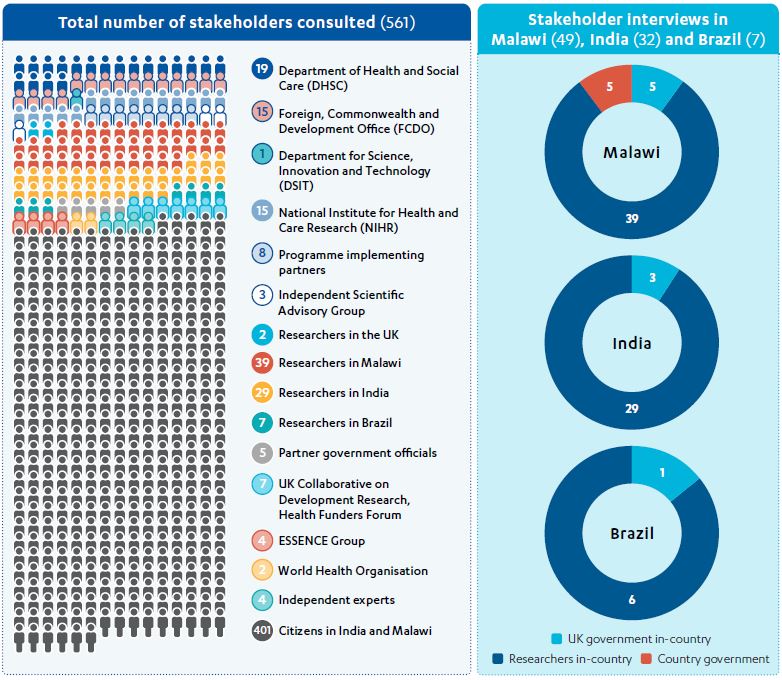
2.5 Our methodology and approach were independently peer-reviewed. We provide a full description of our methodology and sampling in our approach paper. Our programme review sample accounts for approximately 73% of DHSC’s actual and forecast global health research expenditure during the period 2018-19 to 2024-25. Our country case studies encompassed low-income, lower-middle income and upper-middle income countries with different levels of health system coverage and of health threat readiness. The three countries also offered the opportunity to look at a range of funded projects within our broader programme sample (see Figure 2). The principal limitations to our methodology are outlined in Box 2.
Box 2: Limitations of the review methodology
- Data on impact: Research commissioning is carried out over long periods of time, with long and complex pathways to impact. Most research projects funded by DHSC ODA have not yet been completed and most findings have not been reported. We could not assess research quality in the time available for this review, which is a critical factor affecting uptake and impact.
- Generalisability of findings: Our country case study project sample represents a relatively small share of the research funded by large and complex programmes.
- Timescale: This review has a shorter timeline than would normally be the case for a full ICAI review because of delays in extending the third ICAI commission, which means that the evidence gathering period was condensed and that different components of the methodology had to run in parallel.
2.6 Evidence gathering for the review was undertaken during the period November 2023 to January 2024. Altogether, we conducted 122 interviews covering 160 key stakeholders, including more than 30 representatives of UK government departments and agencies, and we reviewed more than 1,000 documents. Through our citizen engagement component, researchers in Malawi and India spoke with more than 400 people (see Figure 3).
3. Background
The global context
3.1 The field of global health research has its historical roots in colonial health practice and the concept of ‘tropical medicine’. During the 19th and early 20th centuries, tropical medicine research centres were established in the global North, including the Liverpool School of Tropical Medicine and the London School of Hygiene and Tropical Medicine in the UK. Alongside this, the funding of research units in Africa and Asia, which were linked with research institutes and universities in the global North, created islands of capacity in countries with limited wider infrastructure.
3.2 Within today’s international health architecture, the World Health Organisation (WHO) has among its functions the promotion and conduct of global health research. The Special Programme for Research and Training in Tropical Diseases (TDR), launched in 1975, is co-sponsored by WHO and three other international agencies. It focuses on strengthening research capacity in “disease-affected countries” and translating evidence into practice to reduce infectious disease and build resilience in the most vulnerable populations.
3.3 Despite historical funding and the efforts of TDR, in 1990 an independent Commission on Health Research for Development found a “stark contrast between the global distribution of sickness and death, and the allocation of health research funding”, with less than 10% of health research spending devoted to 90% of the global disease burden. This came to be known as the 10/90 gap. An increase in aid funding for global health research and related capacity strengthening, to 5% of health ODA, was recommended.
3.4 The late 1990s and early 2000s witnessed a proliferation of public-private partnerships and other global health research initiatives designed to close the 10/90 gap. These included the Global Forum on Health Research, the Alliance for Health Policy and Systems Research, and the Drugs for Neglected Diseases initiative, alongside a wide range of disease-specific product development partnerships such as the International AIDS Vaccine Initiative and the Medicines for Malaria Venture.
3.5 The UK played an important role in many of these global health research initiatives and partnerships, primarily through official development assistance (ODA) contributions made by the former Department for International Development (DFID). However, many other UK institutions have also played their part. For example, the Royal College of Physicians hosted a 2012 meeting to agree the London Declaration on Neglected Tropical Diseases, which aimed to control or eliminate ten neglected diseases by 2020 through public and private sector financing of health research and development (R&D). New opportunities for R&D have been created through the work of the Wellcome Sanger Institute to provide the reference genome sequences of all human infectious disease pathogens.
UK aid funding for global health research
3.6 The allocation of UK ODA to global health research remained DFID’s responsibility until relatively recently. DFID’s work in this area included funding to research consortia and product development partnerships, the agreement of research concordats with key institutions such as the Medical Research Council, and the creation of health resource centres focused on evidence for policy and practice.
3.7 The 2015 Aid Strategy signalled a growing role for other government departments in ODA management. The Department of Health and Social Care (DHSC) received its first ODA allocations through the 2015 spending review, as global health security concerns intensified across the UK government and internationally due to the 2014-16 Ebola epidemic in West Africa, and with the O’Neill Review on Antimicrobial Resistance ongoing. Indeed, the 2015 UK Aid Strategy referenced several new global health research initiatives, including the UK Vaccine Network (UKVN) and the Global AMR Innovation Fund (GAMRIF), under its objective on “strengthening resilience and response to crises”. In 2023, DHSC’s ODA spend was the third-largest of all government departments, after FCDO and the Home Office.
3.8 DHSC now manages two global health research portfolios. The first is the Global Health Research (GHR) portfolio. This includes programmes managed through the National Institute for Health and Care Research (NIHR), which was set up to improve the health of the UK through research but from 2016 also took on the task of managing aid-funded research programmes for the primary benefit of low- and middle-income countries (LMICs) (see Box 3). The GHR portfolio also includes NIHR partnerships that are managed by DHSC. The second is the Global Health Security (GHS) research and innovation portfolio, which is managed by DHSC as part of wider departmental and UK government programming to improve health security and health resilience. DHSC also contributes to the Coalition on Epidemic Preparedness Innovations (CEPI). We set out the DHSC ODA-funded research programmes that we sampled across these two portfolios in Table 2 and Figure 2 above. Box 4 summarises eligibility criteria for the use of ODA to fund global health research.
Box 3: The National Institute for Health and Care Research
The National Institute for Health and Care Research (NIHR) is funded by DHSC “to improve the health and wealth of the nation through research” across six core workstreams. NIHR’s boards report to DHSC’s Science, Research and Evidence Directorate, and senior staff have dual roles. The DHSC Chief Scientific Adviser acts as NIHR Chief Executive, for example. NIHR’s funding schemes are managed through its Coordinating Centre.
NIHR’s ODA-funded global health workstream – which is in effect DHSC’s GHR portfolio – was established in 2016, and by the 2018-19 financial year it accounted for almost 10% of NIHR expenditure. NIHR describes its work on global health as having three strands:
- Programmes: researcher-led and targeted thematic research calls, which NIHR directly commissions and manages.
- Partnerships: schemes to fund global health research, which NIHR contributes to or co-creates with other organisations that have a strong track record in this field.
- People: support for research capability, training, and the development of global health researchers and future leaders in the UK and LMICs, including activities delivered through the NIHR Global Health Research Academy. This work cuts across the programmes and partnerships.
During 2022-23, NIHR’s total spend was £1.32 billion, of which £71.6 million was ODA. According to NIHR, this supported research across 53 LMICs. NIHR has now established itself as a major funder of global health research in the UK and internationally.
Box 4: The use of ODA to fund global health research
For health research to be eligible for ODA funding, it must be conducted for the primary benefit of LMICs, in line with the rules established by the Development Assistance Committee of the Organisation for Economic Cooperation and Development (OECD-DAC).
Benefits to LMICs that align with OECD-DAC definitions include:
- Public health or social welfare, for example where research is focused on diseases or health issues that primarily affect people in ODA-eligible countries.
- Health research capacity development, such as training, the sharing of knowledge and intellectual property, and the transfer of technologies.
- Economic development, for example where research is undertaken by institutions in ODA-eligible countries.
3.9 Figure 4 shows actual and projected DHSC ODA expenditure on global health research from the 201819 financial year through to the end of the current spending review period in 2024-25. Within this timeframe, DHSC’s ODA spending and programming has been shaped by several factors beyond its control, including reductions to UK gross national income (GNI) and to the target for ODA as a share of GNI, HM Treasury requests for ODA savings across government, and the sharp increase in the use of ODA to support refugees and asylum seekers in the UK.
Figure 4: DHSC ODA expenditure on global health research 2018-19 to 2024-25
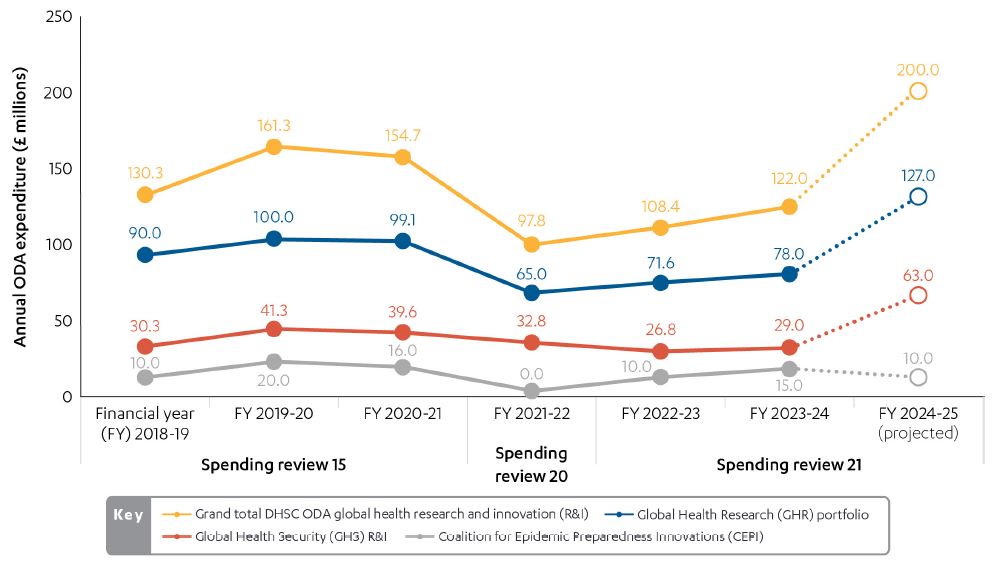
Figure 4 shows actual spend by UK financial year for 2018-19 to 2023-24 and projected expenditure for 2024-25. Projections are indicative and future expenditure may be affected by changing global needs, including humanitarian crises, fluctuations in GNI and other ODA allocation decisions.
Alongside DHSC, the main UK government departments spending ODA on global health research are the Foreign, Commonwealth and Development Office (FCDO) and the Department for Science, Innovation and Technology (DSIT). The UK spends a much larger share of its health ODA on research than other countries, significantly exceeding the 5% recommended to overcome the 10/90 gap. According to the WHO Global Observatory on Health R&D, the UK spent $1.44 billion on health ODA in 2020, of which 33.45% was for “medical research”. In comparison, Germany’s health ODA expenditure was $1.7 billion, with just 3.17% going to “medical research”. After the UK, Belgium spends the greatest share of its health ODA on research (14.71% in 2020).
Within the UK, there are several cross-government ODA governance, oversight and coordination mechanisms for global health research. The UK Collaborative on Development Research (UKCDR) sits outside government and is hosted by Wellcome, its only non-government member. UKCDR aims to map all ODA for research and improve its coherence, including through meetings of the Strategic Coherence of ODA-funded Research (SCOR) Board, which brings together the major UK funders of development research. UKCDR also convenes several research funders’ groups on specific topics, including the Health Funders Forum.
3.12 The UK’s Global Health Framework, agreed in 2023, is a key document aimed at ensuring government coherence in this area, and it includes an objective on research. However, a wide range of UK government strategies are relevant to ODA and other global health research programmes. The principal publications during the period under review are set out in Box 5.
Box 5: UK government strategy and global health research
Since 2018, the UK government has published several strategy documents related to global health research.
The 2021 UK Innovation Strategy stated that UK aid “finances innovation around the world to reduce poverty, stimulate growth, create opportunities for UK business and build trading partners of the future”, while also emphasising the role of innovation in the COVID-19 pandemic response. This was underscored in the 2021 autumn budget, which showed an upward trajectory for total R&D ODA across all departments, rising from £600 million in 2021-22 to £1 billion in 2024-25.
The 2021 Integrated Review of security, defence, development and foreign policy confirmed the spending review 2020 allocation of £1.3 billion to DHSC (ODA and non-ODA) for R&D. It committed to accelerating the development and deployment of vaccines, therapeutics and diagnostics for “emerging diseases”. Global health security was cited as an ODA priority for 2021-22, alongside science and technology.
The 2022 Strategy for International Development stated that the UK will “invest in the research and innovations needed to keep driving breakthroughs in health systems and health security… to respond to the changing burden of disease and health threats, including from COVID-19, antimicrobial resistance (AMR) and zoonoses”. The strategy referred repeatedly to the need to draw on UK expertise, research and technology for development gain.
The 2023 Integrated Review Refresh identified global health as an “area of vulnerability” for the UK, emphasising the importance of “strengthening health resilience at home and overseas”. Objectives include the UK “leading a global campaign on ‘open science for global resilience’, making the case for a secure, collaborative approach to science that ensures low- and middle-income countries have access to knowledge and resources that can support improved resilience”.
The vision set out in the 2023 Biological Security Strategy is that “by 2030, the UK is resilient to a spectrum of biological threats, and a world leader in responsible innovation, making a positive impact on global health, economic and security outcomes”. The document stresses the importance of health R&D throughout. The Oxford-AstraZeneca COVID-19 vaccine features as a case study, which notes the vital importance of long-term funding through UKVN and UK Research and Innovation (UKRI). GAMRIF is cited as an example of UK leadership on AMR.
The 2023 White Paper on International Development outlines the UK’s commitment to champion collaborative global health research with LMICs. It aims to utilise UK scientific expertise to develop new technologies, strengthen health systems, and improve healthcare access worldwide. The White Paper sets out an ambition to expand funding of Southern-led partnerships “to accelerate research and innovation, and to ensure that findings translate into impacts at scale”, and it highlights initiatives such as UKVN and GAMRIF.
The UK government has also published several roadmaps and frameworks, which outline how key strategies will be translated into expenditure and action:
- The 2017 Industrial Strategy committed to spending 2.4% of UK GDP on R&D by 2027, and the 2020 UK Research and Development Roadmap articulated how this target would be achieved. The Roadmap underlined that the UK’s ODA ‘investment’ in R&D “leverages soft-power influence to position the UK as the partner of choice, securing access to future markets, beyond aid”. It framed LMIC capacity strengthening in similar terms: “ODA funds also support the development of researchers and R&D ecosystems in ODA eligible countries – these are our partners of today and for tomorrow”. It referenced 100 Science and Innovation Network officers working across 40 countries to promote UK research and identify opportunities for collaboration, and three UK “science, technology and innovation platforms” in African regional hubs (based in Kenya, Nigeria and South Africa) that “link UK researchers, innovators and entrepreneurs to African policy makers and innovation ecosystems”.
- The 2023 Science and Technology Framework set out the government’s ‘science and technology superpower’ agenda and outlined ten key actions to achieve the goal of becoming “the most innovative economy in the world” by 2030. It also stated aspirations for a UK “diplomatic network with strong science and technical knowledge and in-country networks, and greater international technology leadership”.
- The 2023 Global Health Framework outlined cross-government objectives “to strengthen global health security, reform the global health architecture, strengthen health systems in the UK and globally, and advance the UK’s position as a leader in global health science and technology”, alongside related actions to be taken during the period 2023-25.
4. Findings
Relevance: How relevant are DHSC’s ODA-funded global health research portfolios to the UK’s strategic objectives on global health?
UK government strategies related to global health research have prioritised economic and trade objectives alongside resilience to health threats
4.1 During the period under review, the UK government has generated a wide range of strategy documents related to global health research, a selection of which are set out in Box 5. The government’s science-focused strategies emphasise the need for the UK to build global research and development (R&D) partnerships, with low- and middle-income countries (LMICs) characterised as critical partners for the future. Examples include the 2020 Research and Development Roadmap, the 2021 Innovation Strategy, and the 2023 Science and Technology Framework. Meanwhile, other international strategies stress the importance of funding research and innovation to improve health security and health resilience, within LMICs and globally. Examples include the 2021 Integrated Review and its 2023 refresh, as well as the 2022 Strategy for International Development.
4.2 The more recent White Paper on International Development, which was published in November 2023, emphasises the health needs of people in LMICs and opportunities for UK aid to strengthen research leadership and capacity in these countries. The paper specifically highlights the need for development research to be led by the Global South and for research and innovation partnerships to be equitable, noting that research partnerships based on mutually agreed priorities can have significant development impact.
“Long-term, predictable commitment, secure funding and less bureaucratic open competition would increase the ability of researchers to generate locally relevant high-quality evidence and insights, to inform evidence-based national policy and investments.”
White Paper, 2023, p. 121, link
“We will strengthen our bilateral science and technology partnerships with low- and middle-income countries. We will expand our investments and UK private sector support to southern-led, equitable research and innovation initiatives, tapping into the energy and ambition of early career scientists and researchers.”
White Paper, 2023, p. 123, link
4.3 The government’s Global Health Framework was published in May 2023. It was developed jointly by the Foreign, Commonwealth and Development Office (FCDO) and the Department of Health and Social Care (DHSC), along with three other government departments. It pulls together the themes from other UK strategies in its fourth objective, to “advance UK leadership in science and technology, strengthening the global health research base of UK and partner countries, while supporting trade and investment”. Proposed actions in this area centre on the role of UK science and technology, including in international partnerships for health R&D and in preparations for future pandemics. The Global Health Research Unit on Global Surgery, funded by the National Institute for Health and Care Research (NIHR), is highlighted as an equitable partnership between researchers in the UK and LMICs.
4.4 We found that, during the period under review, DHSC’s global health research programming has remained closely aligned with core UK priorities and interests in building the science base, supporting R&D, and improving global health security.
In developing its ODA-funded research portfolios, DHSC initially focused on complementing the work of other government departments
4.5 When DHSC received its first ever official development assistance (ODA) allocation for research through the 2015 spending review, the department aimed to complement the work of the former Department for International Development (DFID, now FCDO) and the former Department for Business, Energy and Industrial Strategy (now the Department for Science, Innovation and Technology, DSIT) through a focus on global health security, non-communicable diseases, and health issues primarily affecting poor people in ODA-eligible middle-income countries (rather than low-income countries). DHSC launched its Global Health Research (GHR) portfolio in 2016, managed by NIHR. In interviews with ICAI, some stakeholders perceived NIHR’s engagement as an opportunity to involve the National Health Service in global health research, but this has not featured in DHSC’s ODA-funded research programming.
4.6 An early priority within this GHR portfolio was to pivot UK researchers not previously active in this area towards global health, and to ‘level up’ related research funding by engaging a wider range of UK universities through new NIHR awards. The apparent aim was to broaden the range of UK institutions involved in global health research, expanding UK capacity beyond the tropical medicine schools and other universities that had dominated the field.
4.7 In addition to the GHR portfolio managed by NIHR, DHSC also developed a Global Health Security (GHS) research and innovation portfolio. The main objective of this portfolio, referenced in the 2015 UK Aid Strategy and launched the same year, was to address gaps in research identified during the West Africa Ebola epidemic of 2014-16 and through an assessment of the global burden of antimicrobial resistance (AMR). To deliver the GHS portfolio, the department opted to engage expert delivery partners in the UK and internationally.
Over time, the GHR portfolio has broadened considerably
4.8 DHSC’s GHR portfolio has evolved since its inception, and it now covers a wide spread of global health needs and challenges. Many of the portfolio’s newer areas of research fill gaps: for instance, there is now research on some neglected tropical diseases. DHSC has also extended its GHR portfolio to include researcher capacity strengthening and communicable disease research, for example to address COVID-19. Several stakeholders highlighted DHSC’s support for research topics that are underfunded internationally, such as accidents and injuries, as well as the department’s strong focus on AMR and its funding for vaccine development and clinical trials that cuts across both the GHR and GHS portfolios.
4.9 The broadening of DHSC’s GHR portfolio has encompassed areas of FCDO strategic and programmatic focus such as mental health and health systems, leading to greater overlap. FCDO and DHSC have sought to clarify their respective roles and areas of collaboration, including through a 2022 presentation to the Strategic Coherence of ODA-funded Research (SCOR) Board managed by the UK Collaborative on Development Research (UKCDR), which covered UK government coherence on global health research. Stakeholders told us that, to avoid duplication with NIHR awards, the Medical Research Council (MRC) has withdrawn its own health systems research funding scheme. DHSC has sought to limit overlap and increase coherence by joining pre-existing partnerships, such as the Joint Global Health Trials Initiative (JGHT), which it now co-funds with the MRC, FCDO and Wellcome. Other partnerships have been co-created in response to emerging priorities, including the Global Effort on COVID-19 (GECO) Health Research, which was developed by DHSC, NIHR, and the MRC under UK Research and Innovation (UKRI) to address areas highlighted in the World Health Organisation’s (WHO) coronavirus research roadmap. In interviews with ICAI, several stakeholders commented on the increased breadth of DHSC and NIHR programming, perceiving a lack of focus or comparative advantage. Some stakeholders also raised the question of whether NIHR’s initial narrow remit had made it more difficult to spend their ODA allocation.
DHSC’s ODA-funded research in LMICs is generally relevant to key health challenges in these contexts
The country case studies and the citizen engagement for this review confirmed the general relevance of both the GHR and GHS portfolios to the health challenges experienced in these contexts, including those that are stigmatised or underfunded. For example, we engaged with researchers working on cutaneous leishmaniasis in Brazil, LGBTQIA+ wellbeing in India, and multi-morbidity in Malawi. The research projects funded through DHSC ODA are focused on identifying and testing appropriate solutions to health issues that disproportionately impact LMICs, often with practical application in clinical or community settings. For instance, in both India and Malawi, ICAI met with teams assessing interventions to improve neonatal care. Some country-level studies form part of longer-term initiatives such as multi-country clinical trials.
4.11 However, ICAI’s citizen engagement research in India and Malawi identified additional community-level priorities that are not well represented in DHSC portfolios. These include longstanding health system challenges such as access to medicines and the quality and affordability of care, and social and environmental determinants of health such as nutrition, water and sanitation. Health systems research is traditionally a stronger feature of FCDO’s research portfolios, although it is now also supported by DHSC. Focus group participants in both countries, when asked about the most pressing community health priorities, often mentioned that although healthcare facilities exist, they do not provide poor community members with access to appropriate and affordable medicines and diagnostic tests.
“The facilities are available, and most people have access to them, but the problem is usually the same, the lack of drugs. And a lot of people here cannot afford to pay the fees that are charged in the private facilities.”
Man, Lilongwe, Malawi
“The private clinic has helped to ease the problem of accessibility, yes, but at what cost? Too many medications given, sometimes wrong.”
Woman, Lilongwe, Malawi
Another frequently raised topic was that poor members of the community often do not receive the respectful and professional healthcare that they need.
“No ambulance came here. I was transported in an E-rickshaw. Even at the hospital, I lay on the bed, screaming in pain, and eventually delivered the baby without medical assistance. The nurse only arrived to cut the cord. No family member was allowed inside, and my pleas for help went unanswered.”
Woman, Sonia Camp, Delhi, India
“My grandson was sick and was turning blue. We took him to [a government hospital], but they didn’t even test him and told us that he had taken contaminated water and would be fine and asked us to take him home. We requested and begged there but no action was taken and later that evening I brought back the dead body of my nine-year-old grandson.”
Man, Sonia Camp, Delhi, India
“The diagnosis of serious ailments is very poor here. Doctors don’t pay attention to patients and hustle through. Our father had cancer, and the hospital kept treating him for TB. Cancer was diagnosed in Rohtak and by then he already had reached the severe stage, and he suffered a lot during his last days.”
Woman, Panipat, India
Finally, focus group participants in both countries highlighted that public health is not only about medical treatment and access to facilities, but also hygiene and nutrition. This point is also made in the academic literature on best practice in global health research, which emphasises the holistic and multidisciplinary nature of global health challenges.
“They [Malawian health authorities] may give us messages on how to prevent getting cholera, but still we are poor here and many times we lack food, and we are forced to eat food that may not be safe to eat. In that regard we still end up getting cholera, and we have lost family members before because the distance to the hospital was too great.”
Man, Dedza, Malawi
“They [Indian health authorities] think it’s our fate to be born in filth and live in it till we die, [so] why would they bother?”
Man, Panipat, India
4.12 The community members contributing to ICAI’s focus group discussions raised issues that are likely to affect many poor people in ODA-eligible middle-income countries, a priority population for DHSC’s global health research programming, as well as those in low-income countries. While ICAI found that DHSC’s ODA-funded global health research in India and Malawi is relevant to health needs in the two countries, ICAI’s citizen engagement research highlights the many barriers to good health that the poorer communities within the two countries continue to face.
DHSC takes account of global expert views when scoping new areas of programming, but has no process for engaging with the research priorities of LMIC governments
4.13 In December 2021, DHSC commissioned an evaluation of its GHR portfolio, which has recently concluded. The portfolio-level evaluation found that more needed to be done to engage with LMIC policymakers at the design stage of GHR programmes and projects. ICAI’s own research found that this applied equally to the overall design of both the GHR and GHS portfolios. The GHS research and innovation portfolio is part of a wider UK government effort to strengthen global health security, preparedness and resilience, which is led from Whitehall and influenced by UK engagement with key international partners, including in fora such as the G7. The GHR portfolio is informed by DHSC involvement in the UKCDR, including its Health Funders Forum. DHSC also serves on the Steering Committee of ESSENCE (Enhancing Support for Strengthening the Effectiveness of National Capacity Efforts) on Health Research, an initiative among international funders to strengthen donor harmonisation and alignment of investments in research capacity. Its working groups have limited LMIC representation.
4.14 DHSC has established an Independent Scientific Advisory Group (ISAG), which influences the overall shape of the GHR portfolio and the scoping of GHR programmes. This group has strong LMIC expert participation, and its members told ICAI that DHSC and its delivery partners listen to and act upon ISAG views. There is no equivalent portfolio-level forum influencing GHS programming. However, DHSC has sought expert input when scoping individual GHS programmes. For example, an expert panel made recommendations on the priority pathogens for the UK Vaccine Network (UKVN) programme and this work was later published. To develop the Global AMR Innovation Fund (GAMRIF), DHSC drew heavily on the O’Neill Review and the recommendations of UN agencies.
4.15 Unlike FCDO, DHSC is not in a position to deploy staff abroad. In India, FCDO science and health advisers are supporting both ODA and non-ODA programming to develop UK-India research partnerships. DHSC also told us about its engagement with FCDO health advisers during several visits to Bangladesh. Aside from this, ICAI found that DHSC had little engagement with UK embassies and FCDO health advisers, who generally lack the capacity to support ODA-funded programmes managed by other government departments. This lack of interface limits the opportunity for DHSC to connect its global health research portfolios with LMIC government priorities and national health research plans, or with FCDO’s bilateral programming and the work of other development partners. We also heard from global and country-level interviews that many national research ethics committees approve all applications to conduct research within their country context, which suggests a lack of agency or capacity. Some LMIC researchers told ICAI that their projects would not have progressed without external support, due to a lack of interest or funding from national ministries of health.
4.16 Engagement with governments and other stakeholders in LMICs is generally researcher-led, with discussions focused on specific projects or undertaken within the context of wider institutional relationships. For example, ICAI documented evidence of longstanding collaboration between the Malawi Liverpool Wellcome (MLW) programme, the government of Malawi and other national institutions, including the principal hospitals and medical training centres. The MLW Policy Unit meets regularly with the Ministry of Health to discuss research project design, findings, and potential impacts.
“MLW respects community structures, and they really try to inform people in an orderly manner of what they are doing. The staff are easily recognisable as they all have proper identification. They have a good rapport with the community through involving chiefs, the HAC [health advisory committee], and us as CAG [MLW institutional community advisory group] and CAB [project-level community advisory board] members.”
Community advisory board member, Multilink project, Malawi
4.17 Project-level engagement with LMIC governments may also occur through community engagement and involvement (CEI) approaches, which have been rolled out across NIHR’s ODA-funded schemes. CEI allows LMIC stakeholders, communities and healthcare users to share their perspectives and inform research on an ongoing basis, particularly during project implementation. In some cases, government is represented within these project-level community advisory groups.
DHSC references ‘equitable partnerships’ as a principle guiding the development and implementation of its ODA-funded research
4.18 DHSC uses the definition of equitable partnerships set out in Box 6 below, which was developed by UKCDR. In discussion with ICAI, stakeholders stressed that equitable partnerships are dependent on research capacity strengthening in LMICs. This connection is made in UKCDR’s guidance, particularly in relation to institutional capacity. UKCDR also notes the importance of inclusive agenda-setting processes, equitable budgets, and engagement with LMIC governments (see Box 6). Within DHSC’s GHR portfolio, this is echoed in NIHR’s guidance to applicants. The NIHR website lists resources from UKCDR and elsewhere, steering research applicants towards actions that support equitable research partnerships. NIHR Call Guidance includes equitable partnerships as a key selection criterion, although specific requirements vary across programmes and across different calls within programmes.
“We expect equity to be strongly reflected in research leadership, decision-making, capacity strengthening, governance, appropriate distribution of funds, ethics processes, data ownership, publication and dissemination of findings.”
Build equitable partnerships, NIHR website, link
4.19 The GHS portfolio-level theory of change also lists ‘equitable partnerships’ as a principle. The theory of change itself has no supporting detail, but a corresponding narrative briefly explains what is meant by equitable partnerships. At GHS programme level, treatment of the concept varies widely. For example, the UK Public Health Rapid Support Team (UK-PHRST) theory of change commits to research being “equitably identified and delivered” and this is reflected in the programme’s strategic framework for 2022-25, which emphasises “mutual participation” and the value of regional and national partners’ knowledge, expertise and cultural insights. In contrast, the initial UKVN theory of change focused on the UK as a location for vaccine research and manufacturing, while the original business case highlighted other high-income countries and international organisations as potential partners rather than LMICs. The theory of change is being modified for UKVN phase 2, but actions to enable greater LMIC involvement in either vaccine research or manufacturing innovation are limited.
Box 6: What do equitable research partnerships look like?
DHSC has adopted the UKCDR definition of equitable research partnerships: “Partnerships in which there is mutual participation, mutual trust and respect, mutual benefit and equal value placed on each partner’s contribution at all stages of the research process”.
In a related briefing note, UKCDR outlines how research funders can put the principles of equity and mutuality into practice. Suggestions include mandating inclusive agenda-setting, setting equitable budgets, diversifying partners and networks, supporting institutional capacity strengthening, and offering long-term investment. The briefing also underscores the need for coordination with other research funders and for communication with ministries and agencies in the countries where research is conducted.
Despite recent progress, the department’s approach is not yet delivering equitable partnerships across all areas of activity in line with the UKCDR definition
4.20 Data on equitable partnerships are not consistently collated for the GHR and GHS portfolios. When requested, DHSC provided ICAI with data on key metrics for NIHR core programming but not for all NIHR partnerships, nor for the GHS portfolio. Therefore, we do not have a clear picture of the progress DHSC has made in translating its principle of equitable partnership into practice.
4.21 The majority of active research projects funded through NIHR awards, including most Global Research Professorships to date, are led from the UK. Most of these projects engage LMIC partners in joint lead investigator, co-investigator or other research roles. When the NIHR partnerships are considered, the balance between UK and LMIC leadership across the GHR portfolio is much better. All national arms of multi-country studies have LMIC leads. However, some country-level studies have short timescales and limited budgets relative to those of UK leads. Four LMIC research teams that ICAI met in India and Malawi expressed concern about the size of their country-level studies.
4.22 Greater efforts have been made recently to enhance equity by making it easier for LMIC researchers to participate in all project phases. For example, NIHR has made awards of up to £10,000 available to support proposal and partnership development by UK and LMIC researchers between the two application stages of the Research and Innovation for Global Health Transformation (RIGHT) programme. The Global Health Policy and Systems Research (Global HPSR) programme applied learning from this to its first call, offering larger Development Awards to enable joint lead researchers in the UK and LMICs to build partnerships, undertake needs assessments, and identify LMIC research priorities. DHSC policy allows NIHR to extend awards in time and cost so that projects can undertake follow-on activities, such as secondary data analysis to answer new research questions arising from their original work, as well as for additional research dissemination and uptake activities. This policy was recently amended so that extensions for dissemination of research findings can cover LMIC salaries.
4.23 For NIHR core programmes, 2022 data indicate that funding to UK and LMIC institutions is now roughly equal, but with many more research and support staff based in LMICs. This may reflect differences in purchasing power, but it could also indicate a hierarchy or imbalance in some awards, with leaders and senior researchers based in the UK and more junior staff based in LMICs.
4.24 We found that there has been a shift over time towards facilitating greater LMIC leadership of research projects, consistent with the ambition set out in the recent White Paper on International Development. New funding opportunities announced in May 2024 mean that, for the first time, all of NIHR’s global health research schemes will be open to lead researchers from LMICs. The shift towards promoting LMIC leadership has been noticed by LMIC partners, particularly in India. Within both the GHR and GHS portfolios, programmes have evolved to offer direct awards to LMIC institutions. For example, UKVN recently dropped the requirement for a UK lead for one of its calls, although the response from LMIC researchers has so far been modest. Recent calls under the RIGHT programme have attracted roughly equal numbers of proposals from UK and LMIC institutions, although few LMIC applicants have been successful. This may indicate a need for process adjustments or further applicant guidance and support. Other programmes have been more successful, for example Grand Challenges Canada’s Global Mental Health programme, which is maximising LMIC relevance and direct granting to LMIC institutions (see Box 7). Indeed, some schemes, such as the Royal Society of Tropical Medicine and Hygiene’s small grants and early career grants, are open only to LMIC applicants. Stakeholders told us that NIHR could do more to clarify and share good practice on equitable partnerships, and to monitor its application across all GHR programmes.
4.25 ICAI found that the DHSC principle of equitable partnerships is not yet embedded across all areas of global health research activity. For example, there has been some improvement in engaging LMIC researchers in learning activities and events, but this is not yet consistent. At the NIHR’s inaugural GHR portfolio sharing event in 2023, all the presentations were made by UK-based researchers. NIHR launched a global health research journal in early 2024. This journal does not have its own editorial board and there are no experts from LMICs involved in the editorial team for NIHR’s journals. DHSC has said that this oversight will be addressed later in 2024.
4.26 LMIC researcher voices are largely absent from project and programme reporting, and there are limited feedback loops from LMIC communities and stakeholders to DHSC, even where CEI approaches are used. For the recent GHR portfolio-level evaluation, a survey was conducted that gave non-LMIC and LMIC researchers an opportunity to share their perspectives confidentially. This revealed divergent views on equity within NIHR-supported research partnerships, with 90% of non-LMIC researchers saying all partners are involved in equitable decision-making, a view shared by just 66% of LMIC researchers. Similar patterns were seen in questions about the distribution of resources (88% of non-LMIC respondents thought this was fair, versus 60% of LMIC respondents) and benefits (94% versus 74%). This indicates room for improvement, particularly if NIHR and DHSC wish to align fully with the UKCDR definition and guidance on equitable partnerships.
Box 7: Global Mental Health programme
The Global Mental Health programme, managed by Grand Challenges Canada and funded in part by DHSC through NIHR, supports affordable and accessible innovations to address mental health in LMICs, particularly among young people. By inviting applications from and providing grants directly to organisations based in LMICs that focus on community-based mental health services, the programme supports projects that are context-specific and address LMIC needs and priorities. To date, Grand Challenges Canada has supported 124 projects across 42 countries (of which 21 projects across 16 countries have been funded by ODA from DHSC). The majority of these involved the use of seed funding to test interventions with the potential to be scaled up. In India, ICAI visited a project providing safe spaces for LGBTQIA+ young people to meet and discuss their mental health. Their grant had enabled them to trial this approach with students from local colleges.
DHSC has not made any specific commitments to untying its aid for global health research, and its approach to doing so seems inconsistent
4.27 The UK and other members of the Organisation for Economic Cooperation and Development’s Development Assistance Committee (OECD-DAC) have agreed to untie their aid, meaning that ODA funding does not come with an obligation for LMICs to use it to procure goods and services from the respective donor country. The OECD-DAC notes that: “Untying aid – removing the legal and regulatory barriers to open competition for aid funded procurement – generally increases aid effectiveness by reducing transaction costs and improving the ability of recipient countries and territories to set their own course.” The OECD-DAC’s rationale for aid untying echoes good practice for the funding of global health research. For example, it states that untying aid can help donors “foster co-ordinated, efficient and effective partnerships with developing countries”, “strengthen the ownership and responsibility of partner countries in the development process” and promote partner countries’ “integration into the global economy”, while “maintaining a basic sense of national involvement in donor countries alongside the objective of calling upon partner countries’ expertise”.
4.28 DHSC has not focused specifically on untying its aid, in the sense of opening up funding calls to global competition, including from other high-income countries. The department does not systematically track the share of its ODA that flows to specific countries. There are no comprehensive data on how DHSC’s ODA-funded global health research has involved institutions in other high-income countries besides the UK, and data on LMIC institutional engagement and funding flows are only collated for the GHR portfolio. Until late 2020, NIHR was unable to issue contracts to entities outside the UK, whether these were in high-, middle- or low-income countries. NIHR also appears comfortable with UK institutions being the only high-income country leads engaged through its programming. This reflects the UK’s strategic objective to become an R&D superpower (see Box 5). However, it limits the ability of LMIC institutions to choose their partners and is therefore at odds with what the OECD considers better practice. DHSC is working to change this, in line with the White Paper aspiration to increase ‘southern’ leadership in global health research. An overly UK-centric approach also risks missing opportunities to leverage third-party support and to access global partnerships.
4.29 Among DHSC programmes, the Global AMR Innovation Fund (GAMRIF) offers the best example of aid untying. Delivery partners are carefully chosen based on funding criteria that prioritise: selecting the best science, wherever that may be found, to meet global health needs; and opportunities for leveraging additional investment from other funders (see Box 8). For instance, CARB-X funding rounds are open to applicants in any high-income country (HIC) or LMIC, and the initiative can draw on resources from other funders besides GAMRIF where research is not ODA-eligible but remains a high priority for global efforts to tackle AMR. The global BactiVac network facilitates collaboration between academics, industry and policymakers to support the development of vaccines against LMIC-relevant bacterial infections. It has both HIC and LMIC members and offers small catalytic grants. In practice, given the level of infrastructure required, most lead applicants to both CARB-X and BactiVac are from HICs rather than LMICs, but they are not necessarily from the UK.
Box 8: GAMRIF’s international delivery partners
The Global AMR Innovation Fund (GAMRIF) supports research and innovation to address the burden of AMR in LMICs. The first phase of the programme comprised seven work packages delivered through a wide range of international partners:
- Two bilateral partnerships supporting collaborative research with middle-income countries, namely the UK-China ‘Innovation and Collaboration to tackle antimicrobial resistance (AMR)’ project delivered through UKRI (Innovate UK), and the UK-Argentina ‘Tools to tackle AMR in the Environment’ project delivered through two UK research councils.
- Three global research initiatives supporting product development research:
- ‘Accelerating Antibacterial Innovation’ through the Combating Antibiotic-Resistant Bacteria Biopharmaceutical Accelerator (CARB-X) based in the US.
- ‘InnoVet AMR: Innovative Veterinary Solutions for AMR’ through the International Development Research Centre (IDRC) based in Canada.
- ‘Vaccine Innovation’ with BactiVac, a global bacterial vaccinology network coordinated by the University of Birmingham in the UK.
- Two global product development partnerships, through which non-profit organisations work with product developers to bring affordable and accessible health technologies to market in LMICs. GAMRIF supported the ‘Innovation in AMR Diagnostic Tools’ project with the Foundation for Innovative New Diagnostics (FIND), and the ‘New Antibiotic Treatment for Drug-Resistant Gonorrhoea’ project with the Global Antibiotic Research and Development Partnership (GARDP).
As the programme has progressed, DHSC has increasingly identified international delivery partners that have experience in how to engage successfully with LMICs and how to enhance capacity building, access new networks, design equitable partnerships and secure additional funding. For example, GARDP has set up an India Advisory Group to address these areas within the Indian life sciences and pharmaceutical sectors specifically. GAMRIF also tracks funds leveraged from third parties as a key performance metric, with GAMRIF phase one reported to have leveraged £56.5 million from other funders, such as the Bill & Melinda Gates Foundation and the Canadian International Development Research Centre (IDRC), against a UK budget of £63.5 million.
4.30 Throughout ICAI’s discussions with DHSC and NIHR, the concepts of ‘aid untying’ and ‘equitable partnerships’ were conflated by interviewees who almost always responded to questions about untying aid with examples of equitable partnerships between UK and LMIC institutions, and of direct funding to the latter, not of global untying. Specifically, DHSC considers it has untied its ODA through its efforts to increase the share of research funding going to LMIC institutions, and particularly its recent shift towards funding some of those institutions directly, as LMIC lead applicants for NIHR awards can choose who they wish to partner with globally. However, programme-level approaches are inconsistent. For example, UKVN required a UK lead institution for its projects until very recently. The RIGHT programme also required a UK lead for its first three calls, but with incremental shifts towards greater LMIC engagement over time, and from Call 4 onwards LMIC institutions have been able to apply for RIGHT awards directly. Among the NIHR partnership programmes, the Joint Global Health Trials Initiative (JGHT) and Global Effort on COVID-19 (GECO) Health Research have no requirement for a UK lead, whereas applicants to the Global Mental Health programme must be based either in Canada (effectively tying some aid to this donor country) or in an LMIC.
4.31 It is not clear how DHSC follows OECD guidelines on ensuring best value for money in ODA expenditure. GAMRIF arguably does this by taking an international approach, but for programmes that tie aid to UK researchers, the value for money implications of imposing this limitation do not appear to have been considered.
DHSC programming is generally well aligned with ODA eligibility criteria related to LMIC primary benefit
4.32 DHSC has invested significant resources in understanding ODA eligibility and what it means for global health research as well as upskilling key delivery partners on this issue. ICAI heard that NIHR went through a steep learning curve in relation to managing and safeguarding ODA funds, and in orienting its systems and processes to deliver research in and for LMICs. DHSC worked closely with FCDO’s ODA eligibility team to improve its own knowledge and to support NIHR effectively, including in undertaking visits to LMICs at an early stage in the development of the GHR portfolio.
4.33 We found that DHSC and its delivery partners have put in place appropriate mechanisms for screening potential research programmes and projects with respect to their eligibility for ODA funding. These include the scoping and drafting of detailed spending review bids that set out the strategic rationale for the department’s ODA allocation, business cases for new GHS programmes, and GHR programme development papers. Within the context of each NIHR funding round or call, project proposals are screened for ODA eligibility and for the relevance of the proposed research to the health and development needs of LMICs, before applications can progress further. Similar processes have been put in place for funding calls under GHS programmes.
4.34 Within its core funding schemes, NIHR relies on awardee self-reporting and the cross-checking of financial transactions against original budget proposals, as the main mechanisms for monitoring ongoing ODA eligibility once a research project is launched. There appears to be less emphasis on monitoring the relevance of research outputs and outcomes to LMIC primary benefit and to broader global health objectives.
Financial reporting requirements are particularly burdensome and could undermine DHSC efforts to develop equitable partnerships and strengthen LMIC research capacity
4.35 DHSC has put in place a complicated governance and oversight structure to manage its ODA allocation, expenditure and related programming. This includes numerous DHSC and NIHR committees, boards and groups. Meeting agendas and minutes seen by ICAI recorded discussions dominated by transactional detail in areas such as ODA forecasting and underspends, the potential for savings, currency fluctuations and inflationary pressures, all important for good financial management.
4.36 DHSC concerns about due diligence and the importance of fraud prevention across its global health research portfolios were increased by a 2018 internal audit that highlighted such risks. ICAI agrees that fraud prevention is important. However, we were told by researchers that NIHR controls appear to have resulted in excessively burdensome financial reporting requirements for projects funded through its core programmes, compared to other funders of health research. This was also highlighted by the recent GHR portfolio-level evaluation. ICAI found that award-holders are struggling, despite some capacity strengthening in this area. Researchers in both the UK and LMICs expressed challenges and frustrations, some vehemently. We were told of significant delays in financial transactions and reports being approved, with correspondingly slow reimbursement of costs, and knock-on effects in other areas such as staff recruitment and the agreement of contracts.
4.37 These onerous requirements risk undermining NIHR’s capacity-strengthening efforts, due to the amount of researcher time spent on project administration and reporting. Such requirements also increase the need for institutional capacity development in financial management and reporting, particularly within LMICs. They may put off new or repeat applicants, undermining attempts to diversify award-holders and to strengthen LMIC leadership. In discussion with ICAI, NIHR acknowledged that its ODA monitoring and reporting processes are complex and burdensome, particularly for LMIC institutions. NIHR suggested that requirements could be streamlined in future, at least for smaller awards.
Conclusion on relevance
4.38 We award DHSC a green-amber score for relevance, in recognition of the department’s efforts to complement other funders of global health research and to address topics that are underfunded relative to the illness, injury and death they cause. DHSC is attentive to ODA eligibility and takes ODA management seriously. The department is also working to improve LMIC access to its funding schemes. Its research partnerships are not, however, consistently equitable and much of its research ODA remains tied. Finally, NIHR’s onerous reporting requirements are disproportionate and risk hindering LMIC participation in research funded through the GHR portfolio.
Effectiveness: How effectively does DHSC’s ODA-funded research contribute to improving global health outcomes?
DHSC-funded global health research projects are aimed at improving health practice and ultimately health outcomes, although project-level monitoring primarily captures activities and outputs
4.39 In comparison to ODA-funded research previously reviewed by ICAI, such as the Newton Fund and the Global Challenges Research Fund, DHSC’s portfolios have a stronger focus on generating benefits for people in LMICs and greater potential for impact. As noted in ICAI’s synthesis of review findings from 2019 to 2023 and in paragraph 1.5, one of the first COVID-19 vaccines to receive a WHO Emergency Use Authorisation was developed at Oxford University with UKVN support, building on earlier research into a vaccine against the Middle East Respiratory Syndrome (MERS) virus. DHSC-funded research in Malawi has also contributed to the development of a new typhoid vaccine, which is showing impressive results in efficacy trials. ICAI visited other research projects in Malawi that offer the prospect of shaping health practice in areas such as neonatal care, respectful maternity services, and the management of vectorborne diseases. Potentially valuable innovations are already emerging from these projects, including a neonatal care app. Meanwhile, the ENHANCE project funded through RIGHT, which is assessing a cognitive therapy-based intervention for perinatal depression in Pakistan, was cited in Nature Medicine as one of “11 clinical trials that will shape medicine in 2024”. Several projects ICAI visited in India were based within government health facilities or research institutes, enhancing the likelihood of research findings informing changes to clinical guidelines or health policy.
4.40 Programmes that support discovery research and early-stage product development, such as UKVN and GAMRIF, have longer pathways to impact. Innovation that is intended for the primary benefit of LMICs may also face significant barriers to commercialisation and uptake. Nevertheless, through its GHS portfolio, DHSC backs innovations with strong potential for public health benefit. In India, ICAI visited an impressive small enterprise supported by GAMRIF through CARB-X to research novel treatments for multi-drug-resistant bacterial pneumonia. GAMRIF also provided funding to the Global Antibiotic Research and Development Partnership (GARDP) to support the late-stage development of Zoliflodacin, a new oral treatment for gonorrhoea.
4.41 Most DHSC global health research programmes and projects have not yet concluded or reached the stage where the quality of findings can be gauged. For example, only one project from RIGHT Call 1 has concluded, and across all NIHR awards the majority of projects have needed no-cost extensions, primarily due to the impact of the COVID-19 pandemic. It is therefore too soon to see widespread pull-through of research findings or results into health policies, guidelines, standards, or product uptake. Most programme annual reviews rely mainly on monitoring quantitative data related to research outputs, such as the number of journal articles completed and conference presentations delivered, in addition to documenting project-level research activities.
NIHR’s approach to community engagement and involvement is innovative and its use can open opportunities for localised benefits
4.42 NIHR has applied its experience of funding UK research to the development of applicant guidance for its global health research schemes. Most notably, NIHR drew on the practice of patient and public involvement and engagement in UK research when developing expectations around project-level collaboration with affected communities in LMIC settings. NIHR guidance in this area, known as community engagement and involvement (CEI), is broad and not prescriptive, leaving researchers to determine which groups to engage with and how, depending on the design of each particular project and the LMIC context in which the research takes place.
4.43 The RIGHT programme piloted the use of CEI, and it is now a core requirement for all global health research funded through NIHR. GHR programmes, including RIGHT and Global HPSR funding calls, require CEI plans to be articulated in stage 1 applications, which are formally assessed in stage 2, thus helping to inform the implementation of successful proposals. ICAI’s citizen engagement research in Malawi consulted two community advisory groups that have informed the design and delivery of research activities as well as supporting patient recruitment and community outreach.
“MLW [the Malawi Liverpool Wellcome programme] really takes our views into account, and they try to change things so that as community people, we should be comfortable with health research.”
Community advisory group member, Malawi Liverpool Wellcome, Malawi
The GHR portfolio evaluation noted that researchers had improved their understanding of community-level needs and challenges through CEI. Researchers interviewed by ICAI, including during country case study visits, indicated that they would not have engaged people in this way without NIHR encouragement, a sentiment echoed in DHSC’s recent roundtable discussions with researchers in Bangladesh, Ghana, India and Kenya.
4.44 We found some evidence of localised benefits arising from CEI. For example, in Brazil, one project’s CEI activities led to the production of a film that was shared regionally, to raise awareness about a stigmatising skin condition. Members of the Malawi Liverpool Wellcome institutional community advisory group have supported research to develop a new typhoid vaccine, including through health promotion activities such as discussing typhoid symptoms and the importance of vaccination with local chiefs and school headteachers. In India, the ARTEMIS project has engaged young people as expert advisers on mental health, involving them in awareness-raising activities in ways that also benefit them personally.
“My friend took me to Balika Trust and from there I joined the ARTEMIS group. I am confident in what I do now. I have an awareness now to manage my mental health… We will do a social media campaign in a new project where we want to reach out to a larger mass with our stories and de-stigmatise mental health.”
Member of adolescent expert advisory group, ARTEMIS project, India
“The diagnosis of mental health is also very critical as most people don’t understand the reason why a child is behaving in a certain way. They keep saying that he just needs attention or it’s just a phase. Once identified as a mental health issue, they declare the person mad and start bullying them and their family.”
Member of adolescent expert advisory group, ARTEMIS project, India
In Liberia, peer support groups formed to work with a RIGHT-funded research project are evolving into an independent civil society organisation to continue their advocacy, and some projects have engaged policymakers directly through CEI activities. More generally, the GHR portfolio evaluation found that CEI has helped researchers to identify research dissemination opportunities and change pathways. However, sensitivity is required to tailor CEI approaches appropriately in countries where civil society is restricted. This is an area where FCDO social development, governance and health advisers could usefully provide advice.
Many programmes lack detailed results frameworks, and approaches to impact reporting vary
4.45 We found variation in how results frameworks are developed and used across the DHSC global health research portfolios. Within the GHR portfolio, programmes were originally expected to use the portfolio-level theory of change, which provides the frame of reference for assessing and evaluating programme effectiveness. Alongside this, the portfolio-level results framework offers a ‘standard data and indicator set’ against which all GHR programmes should report. However, such reporting has been inconsistent, particularly across the NIHR partnership programmes. Furthermore, some outcome indicators related to research impact remain optional, and none of the indicators have corresponding targets or milestones. Logical frameworks (logframes) are commonly used to design, plan, monitor and evaluate UK aid programmes. However, DHSC does not use them for GHR programmes, and the department does not appear to set programme-specific targets and milestones.
4.46 Programme-specific theories of change have been developed recently, although those for the RIGHT programme and the Global Research Professorships remain in draft form. At project level, individual research projects funded through the GHR portfolio generally do have their own theories of change, ranging from simple logic chains through to complex narratives. There is wide variability in how projects set targets and milestones, with some using simple timelines, while one GHR Unit has a 94-page monitoring and evaluation framework.
4.47 Within the GHS portfolio, logframes are used at the programme level, but not always meaningfully. For example, UKVN set overly ambitious outputs and outcomes initially, and these specific outputs and outcomes were abandoned for monitoring purposes towards the end of the programme’s first phase. UKVN has since reworked its logframe and theory of change for its second phase.
4.48 Approaches to reporting research outcomes and impact are weak across the two portfolios, and results data are not systematically aggregated at portfolio level to inform assessments of progress. For the GHR portfolio, NIHR has a useful standard operating procedure that guides the production of impact case studies. However, the selection of global health research case studies appears unsystematic across the relevant programmes, and few impact case studies have been written up and published. This lack of available impact stories may provide some explanation for the repeated use of the same programme and project examples across multiple UK strategy documents.
4.49 NIHR’s capacity to develop a more strategic approach to the GHR portfolio and its potential for impact has been constrained by staff turnover and the lack of a GHR programme director. This role has now been established, with the first post-holder appointed in July 2023. Turnover in operational roles continues to be an issue, however, so many NIHR award-holders lack consistent guidance or support with reporting. Some principal investigators said they had dealt with three or four different points of contact for their awards in as many years.
Many programmes indicate a patchy understanding of pathways for evidence translation, which could limit their potential to shape policy and practice
4.50 Knowledge translation can be defined as “ensuring that stakeholders are aware of and use research evidence to inform their health and healthcare decision making”, which drives impact through an “effect on, change or benefit to the economy, society, culture, public policy or services, health, the environment or quality of life”. Where theories of change have been developed for GHR programmes, these mention knowledge translation and exchange, but with few details or examples of how this is realised and sustained. We found an over-reliance on approaches such as Researchfish to report and track the longer-term impact of ODA-funded research, alongside an apparently unstructured approach to the selection and use of impact case studies by both DHSC and NIHR.
4.51 DHSC and NIHR offer limited guidance on research pathways to impact, in comparison to the materials designed to inform CEI activities as well as equitable partnerships and capacity-strengthening efforts. Applicants and awardees are offered little training on impact pathways, and while the RIGHT programme piloted the delivery of applicant webinars on planning for impact, such approaches have not been rolled out. We saw little detailed planning for dissemination and impact at the level of individual research projects. However, NIHR maintains an open access publications policy and offers guidance and support on intellectual property management and commercialisation, to help ensure worldwide access to knowledge and innovation generated through its global health research programmes. This is reinforced through relevant clauses in NIHR’s standard contract for global health research.
4.52 The project-level reporting mechanisms designed by DHSC and NIHR encourage researchers to demonstrate localised and short-term effects, rather than emphasising more complex pathways, most notably those involving evidence synthesis (see Box 9). NIHR funds evidence syntheses that support decision-making across health, public health, and social care in the UK. However, no support has been provided for evidence synthesis in global health, even where DHSC is funding a significant body of research in a particular area through several different programmes, for instance severely stigmatising skin diseases or snakebite. Consideration is now being given to compiling a more limited evidence collection on road accidents, ahead of an international conference on the topic.
4.53 Regardless of whether DHSC funds the work of rigorous evidence synthesis, it could emphasise its importance to GHR award-holders and track the extent to which its ODA-funded research enters these pathways. While inclusion in rigorous evidence synthesis does not guarantee the eventual translation of findings into practice, it indicates potential to contribute to wider impact. An understanding of this could help DHSC to track its contribution to changes in policy and practice and to learn from less successful projects.
4.54 The issues facing GHS programmes are different. DHSC and its partners recognise that many product development projects will be unable to complete clinical development without access to third-party funding, with others failing to be commercialised because of barriers to market entry. Strategies to address this need further development, including closer engagement with potential third-party funders and pharmaceutical manufacturers to obtain feedback that can inform the later stages of product development.
Box 9: The role of evidence synthesis in research impact pathways
In the past, funders of global health research advocated ‘getting research into policy and practice’ (GRIPP), which usually meant attempting to translate the results of each individual study into policy or guidelines. It is now recognised that single studies rarely provide sufficient evidence to effect such changes, that knowledge is cumulative, and that policy should take all relevant research into account through systematic critical appraisal. This is the rationale for evidence synthesis. As a discipline with its own specialist methods, it has expanded rapidly over the past 30 years in response to rising interest and demand, including in global health, and it is now a key element of pathways to impact.
While evidence synthesis can take various forms, rigorous approaches follow a published protocol that specifies the questions to be addressed, a search strategy for sourcing evidence, and criteria for the inclusion of findings in further analysis. Interpretations of evidence should take account of bias, consistency between studies, the size of the effect, and generalisability. In addition to drawing conclusions regarding the state of knowledge on particular questions, such systematic reviews also draw out implications for policy, practice and further research, and usually include non-technical summaries.
Alongside this, methods continue to be developed for communicating research findings to policymakers, generating demand for evidence, and devising guidance for knowledge translation that accounts for feasibility, acceptability and consumer preferences. In many HICs, this work is led by agencies embedded in or contracted by government. In global health, LMICs often look to WHO for leadership, but the need for national capacity in knowledge translation is increasingly recognised. While many systematic reviews are valuable, some are poor-quality or misleading due to the methods used or the positionality of the authors, so those working at the research-policy interface need to be alert to this and stay up to date with the continuously evolving science of evidence synthesis and its use in policy and practice.
Purposive collaboration between DHSC and FCDO is limited, especially in-country, which constrains the potential impact of ODA-funded global health research
4.55 The FCDO health advisory network has limited capacity and is not present in every low- or middle-income country. Meanwhile, the FCDO science network, including its UK Science and Innovation Network (SIN) representatives in relevant countries, focuses on promoting UK interests. We found that DHSC has had little engagement with either network, and it has not made its ODA-funded research portfolios sufficiently visible to FCDO staff based in LMICs. DHSC’s programme information on DevTracker (the FCDO-hosted public aid information portal) is very out of date and inaccurate and the data uploaded to d-portal also have gaps. The UKCDR Mapping ODA research and innovation (MODARI) project aims to capture all research funded with UK ODA, but DHSC data are incomplete there as well. DHSC added new information through a January 2024 update, which also improved the mapping interface, but gaps remain. Specifically, most GHS research and innovation projects were not visible on the MODARI platform at the time of evidence gathering for this ICAI review. Since DevTracker and MODARI are the two key resources that FCDO health advisers and embassies would use to inform themselves of DHSC-funded research projects in a particular country, these data gaps hinder collaboration.
4.56 In India, this information deficit has been addressed by a proactive health adviser working with other FCDO staff to coordinate UK-India collaboration in science and research. ICAI found that British High Commission New Delhi had a good understanding of DHSC’s programming, although there was confusion over whether certain projects were ODA-funded. However, FCDO staff in Brazil and Malawi had very limited awareness of DHSC’s global health research portfolios. This is less of a concern in Brazil, where the SIN is present but there is no FCDO health programming. However, the UK remains a key development partner in Malawi, funding health sector programmes and retaining a small health team.
4.57 Where embassies are not aware of DHSC programming, this increases reputational risk and is likely to result in missed opportunities, for example to share relevant research outputs or to highlight successful partnerships. In Malawi and other countries where FCDO maintains a bilateral health programme, there may be potential to support research uptake. In Malawi, a Global Research Professorship project to develop a neonatal care app was able to access follow-on funding to test the app in primary care settings, through the FCDO Southern Africa Research Hub. The FCDO Malawi health advisers learned about this testing phase and the associated follow-on funding from UN colleagues, rather than from DHSC or NIHR, and they were then able to offer support for scale-up through FCDO’s bilateral health programme.
4.58 The effectiveness and potential impact of innovation programming could be enhanced through ongoing and systematic DHSC engagement with FCDO’s work on product development partnerships, pharmaceutical market-shaping, and access to medicines. Where FCDO and DHSC have collaborated in the past, this has enabled some projects to link up with relevant international partners. For example, GAMRIF helped to connect CARB-X with partners working on access to medicines and related market-shaping in LMICs, such as GARDP and the Clinton Health Access Initiative (CHAI). Such collaboration is also key to identifying options for third-party funding or public-private partnership to take new products to market.
DHSC and NIHR have stated an intent to strengthen individual, institutional and system-level research capacity in LMICs
4.59 NIHR is explicit about the capacity-strengthening aims of its global health research programming, claiming that “NIHR trains and develops future leaders in applied global health research, to support research that improves the health outcomes of people in LMICs. We also strengthen the research capacity of LMICs at individual, institutional and system level.” The GHR portfolio-level theory of change echoes this commitment. It includes activities focused on developing the capacity of researchers and support staff, in both the UK and LMICs. It depicts this individual capacity, equitable research partnerships and thematic networks as outputs that contribute to stronger “LMIC institutional capacity” in the medium term (three to ten years) and to “sustainable growth of the LMIC research ecosystem” over the long term (ten to 25 years). In the GHR portfolio-level theory of change and elsewhere, DHSC and NIHR define a research ecosystem as “researchers and their outputs, research institutions, funders, policy makers who use the research to inform policy, communication specialists who share findings with the public, and private sector companies who develop products and employ researchers”.
4.60 NIHR’s approach therefore appears consistent with the UKCDR definition of research capacity strengthening, which it cites in its guidance to applicants: “Enhancing the ability and resources of individuals, institutions, and/or systems to undertake, communicate, and/or use high quality research efficiently, effectively, and sustainably.” It also captures all three levels of research capacity strengthening described in the good practice document recently published by ESSENCE on Health Research (Box 10). The GHR results framework includes several metrics for individual capacity strengthening, and projects are asked to summarise evidence of institutional capacity strengthening and to record the number of support staff engaged. It is not clear how DHSC’s contribution to system-level capacity strengthening is assessed. Neither the theory of change nor the results framework references the SDG 9 targets or indicators.
Box 10: Strengthening health research capacity in LMICs
A recent ESSENCE good practice document describes three levels of research capacity strengthening:
- “Level 1: The individual level, such as the training of researchers and those that manage research.” Capacity strengthening at this level is “primarily through PhD studentships, post-doctoral fellowships and research management training”.
- “Level 2: The institutional level, such as the physical environment and research culture researchers are working in.” This relates to “physical facilities and resources, staff levels and skills, research systems and cultures of learning and teaching”.
- “Level 3: The national or international level (sometimes called the societal level), such as international collaborations or research uptake systems that individuals and institutions are a part of.” Here, the focus is on “how knowledge is produced, translated and disseminated within and beyond the academy through research uptake, collaborations and networks”. DHSC and NIHR use the term ‘system level’ for this tier of capacity strengthening.
4.61 The GHS portfolio-level theory of change lists capacity strengthening as an output area, with no detail about what this means in practice for research and innovation. Some GHS programmes have indicated their plans in this area. For instance, the UK Public Health Rapid Support Team (UK-PHRST) Research Plan for 2022-25 explores how the programme can further enhance its offer to develop research capacity in partner countries (see Box 11), and the UKVN theory of change for phase 2 references the provision of training and institutional support to LMIC regulators.
Box 11: Enhancing public health research capacity and global health security
The UK Public Health Rapid Support Team is incorporating a wide range of research capacity-strengthening activities into its programming in LMICs. These activities should also contribute to longer-term public health security and health resilience. UK-PHRST’s plans include:
- Expanding collaborations with regional and national public health institutes to support the strengthening of researcher capacity.
- Providing technical training for junior researchers in LMICs in areas such as surveillance methodologies, research design, data analysis and diagnostics.
- Supporting capacity-building projects that develop frameworks and toolkits on sustainable surveillance systems and laboratory capabilities.
- Establishing or supporting user networks and communities of practice that facilitate ongoing learning and quality improvement.
- Sharing standard operating procedures and best practices that support the delivery and management of research in LMICs.
- Supervision and mentoring of LMIC students on research degrees whose work focuses on outbreakrelated or outbreak-prone diseases.
- Ensuring LMIC partners have the opportunity to lead author research publications.
DHSC capacity-strengthening initiatives focus on individuals, with demonstrable impact at this level
4.62 There is a strong emphasis on individual research capacity strengthening within most GHR programmes, consistent with NIHR’s applicant guidance that stresses the need for support to early-career researchers in LMICs. Clear data are starting to emerge on outputs included in the GHR results framework, such as the number of LMIC PhD candidates and how many of these are female. Aggregate data suggest that the number of LMIC candidates funded for postgraduate awards is around ten times the number from the UK.
4.63 Several GHR programmes are designed to support individual capacity strengthening as a primary purpose. These include the NIHR Global Research Professorships, the NIHR-Wellcome Partnership fellowship scheme, and the Royal Society of Tropical Medicine and Hygiene (RSTMH) small grants. However, to date, most successful applicants for the Global Research Professorships have been based in the UK. The new NIHR Global Advanced Fellowship, which will support researchers in postdoctoral roles, has been designed to address a funding gap in the global health research career pathway in both high-income and low- and middle-income countries.
4.64 Other GHR programmes have individual capacity strengthening embedded within them. For example, postgraduate and postdoctoral researcher salaries and training are supported through projects funded under the Research and Innovation for Global Health Transformation (RIGHT) programme, Global Health Policy and Systems Research (Global HPSR), and the GHR Groups and Units. Among the NIHR partnership programmes, the Joint Global Health Trials Initiative (JGHT) has provided training in areas such as electronic data collection and compliance with ethical protocols and international standards. However, neither JGHT nor Global Effort on COVID-19 (GECO) Health Research emphasise individual capacity strengthening. The Global Mental Health programme provides a good deal of training, but this appears to focus on developing mental health professionals and their role in innovation, rather than on fostering research capacity.
4.65 Individuals funded or otherwise supported by GHR programmes to advance their academic careers become members of the NIHR GHR Academy, through which they can access additional training and development opportunities. They are advised and supported by GHR training leads based in the UK and various LMICs. Almost 1,000 people have been aided in this way to date, around 90% of whom are from LMICs. NIHR also offers small awards to support academic career development, such as the GHR Short Placement Award for Research Collaboration (SPARC) scheme, through which NIHR GHR Academy members can access up to £10,000 to design and undertake a short bespoke placement.
4.66 Within the GHS portfolio, UK-PHRST provides teaching and training to junior researchers. Such individual capacity strengthening presents more of a challenge for GHS programmes focused on discovery research and early-stage product development, due to the advanced equipment and technical support infrastructure required to undertake research of this kind. However, some projects supported through GAMRIF have engaged LMIC researchers in work to develop new drugs, vaccines and diagnostics, and the annual reports from GHS programmes document how many LMIC researchers have been engaged in training. For example, UKVN funding to the Vax-Hub project has supported training for 35 individuals working in vaccine manufacture across 15 LMICs.
4.67 ICAI heard that DHSC’s support to individual capacity strengthening in research is welcomed, particularly by early- and mid-career researchers in Brazil, India and Malawi. However, researchers in Malawi also expressed anxiety about how to progress both their research and their careers once their project funding comes to an end, indicating that the individual research capacity built through DHSC’s ODA-funded programmes is at risk of attrition, particularly if there is slow or no growth in institutional and system-level capacity.
Support to institutional capacity strengthening is embedded within some programmes, but is only at the centre of one and is not systematically monitored
4.68 None of DHSC’s GHR or GHS programmes have institutional research capacity strengthening as a primary purpose, although the relatively recent GHR Centres programme (which was not in our sample) has it as one of its main objectives. Some other programmes offer specific support in this area. An example is the financial assurance fund within the GHR Groups and Units, which offers projects awards of up to £50,000 (or £100,000 if shared with other groups or units). These awards can be used to support financial capacity building as well as audits and due diligence checks. NIHR also provided funding via the MRC to the Good Financial Grant Practice programme managed by the African Academy of Sciences, to support the development of a grant management standard and associated assessment tools. NIHR’s broader guidance for global health schemes encourages applicants to include support for training and other activities in areas such as financial management, writing and communications, and CEI, as well as institutional systems for coaching and mentoring. Similar support is provided through some NIHR partnerships, for example the Global Mental Health programme, which conducts risk assessments to identify weaknesses in funded organisations and then helps grantees to address them.
4.69 DHSC has not yet unpacked the pathways between individual and institutional capacity strengthening. However, capacity has begun to extend from the individual to the institutional level, particularly where LMIC partners have more substantial roles in NIHR-funded projects, as ICAI observed in India and Malawi. Some training of individuals may also expand institutional capabilities. For example, UK-PHRST is training LMIC researchers in public health surveillance methodologies, and in India ICAI was shown a suite of laboratories that had been upgraded to conduct AMR surveillance research under an NIHR GHR Unit award.
4.70 In programme-level reporting, institutional capacity-strengthening outcomes and their value are not demonstrated in a systematic way. The GHR results framework prompts project leads to answer broad questions around how their award has supported the development of LMIC capacity and infrastructure, and to report the activities and outcomes that they deem to be most significant. However, most project leads are currently UK-based. No dedicated mechanism is provided for LMIC partners to share their perspective, confidentially or otherwise. GHS programme data and reporting are also very limited in this area, with the exception of UK-PHRST.
DHSC ambitions related to system-level capacity strengthening are unclear
4.71 DHSC ODA to global health research is significant, totalling almost £1 billion during the period under review (2018-19 to 2024-25), and rising to £200 million a year at the end of this period (see Figure 4 in section 3). This scale of funding offers an opportunity to support knowledge sector growth in some LMICs, and to contribute to the realisation of SDG 9 targets on increasing the number of researchers and the level of public and private investment in R&D. However, despite DHSC’s stated intent to build the “LMIC research ecosystem” over the long term, its ambition in this area is unclear, there is no evident planning for its contribution, and the department’s ODA funds are spread widely and thinly, limiting their transformative potential.
4.72 Under NIHR-funded projects, CEI activities could help to strengthen demand for health research as well as public understanding and use of research outputs, consistent with the GHR portfolio-level theory of change. ICAI’s citizen engagement research in Malawi documented how the institutional-level community advisory group set up by the Malawi Liverpool Wellcome (MLW) programme is playing a role in this.
“There are some beliefs that are embedded in the community, especially when it comes to health, such that some people may not always understand when MLW requests to take, say, nose swabs, urine samples, and the like. We are there to ensure that we convince the people that there is no risk in being involved with MLW.”
Community advisory group member, Malawi Liverpool Wellcome, Malawi
“People do not often come to tell me that they are willing to participate, say, in vaccines, but after we have shared information, when people show up and they get, say, the cholera vaccine, I am happy because I know that my information was received positively.”
Community advisory group member, Malawi Liverpool Wellcome, Malawi
Our focus groups with CEI participants in India and Malawi suggest that CEI can also play a capacity-strengthening role for community members.
“We can say that we improved ourselves from here, our confidence and self-esteem improved.”
Member of adolescent expert advisory group, ARTEMIS project, India
“I may not be a medical doctor, but I do know a lot about causes of various diseases and how vaccines and medicines work now.”
Community advisory group member, Malawi Liverpool Wellcome, Malawi
However, NIHR’s current emphasis is on improving research project “reach, quality and impact” through CEI activities, rather than on how community capacity can grow through engagement in these processes. Overall, NIHR’s approach to capacity strengthening is rather narrow and focused on the individual far more than on the institutional or system levels. This inhibits prospects for transformational change, including towards greater LMIC leadership in global health research.
4.73 At a more strategic level, the indicators for capacity strengthening under objective 4 of the UK government’s Global Health Framework (see paragraph 4.3) have not yet been developed. There is also a lack of DHSC guidance, expectations, good practice examples or peer learning related to system-level capacity strengthening.
Conclusion on effectiveness
4.74 We have awarded DHSC’s global health research programming a green-amber score for effectiveness. This reflects the contributions that are already being made to improved health outcomes, most obviously through the development of vaccines for typhoid and COVID-19. Valuable innovations are also emerging in areas such as neonatal health. The scoring recognises DHSC’s innovative use of community engagement and involvement (CEI) to strengthen research projects and deliver localised benefits, alongside its evident contribution to strengthening individual research capacity in LMICs. However, DHSC is not sufficiently deliberate in planning, monitoring and reporting its contribution to strengthening institutional and system-level capacity.
4.75 Despite the scale of DHSC ODA funding for global health research, the full extent of its contribution to improved health practice in LMICs is not yet evident. Few projects have concluded, so it will be some time before findings can be assessed and incorporated into the wider evidence base for policy and practice. Considering the size of its global health research portfolios, DHSC has not sufficiently realised its potential for transformative impact through, particularly, promoting the role of rigorous evidence synthesis. DHSC-funded researchers are engaging with policymakers and other stakeholders in LMICs, including through CEI activities, which may foster interest in research outputs and eventual uptake. However, some projects will need to access third-party funding, collaborations or partnerships to advance their innovations.
Learning: Has the design of DHSC’s global health research portfolios been informed by its own monitoring, evaluation and learning, and by lessons from other ODA-funded health research?
DHSC engages proactively in fora that enable the department to learn from other UK and international funders of global health research
4.76 DHSC stakeholders noted the willingness and interest of the department and of NIHR to learn from other UK and international funders of global health research. However, DHSC’s engagement in relevant learning mechanisms through the ESSENCE and UKCDR platforms has been limited to the GHR portfolio. Senior leaders from DHSC’s GHR portfolio participate in a range of UKCDR funders groups, including those on epidemic preparedness and response and on disaster risk reduction that are directly relevant to the GHS portfolio. There has, nonetheless, been some GHS portfolio learning from other funders working on specific topics. For example, the GAMRIF programme has engaged with the Antimicrobial Resistance Funders’ Forum run by the MRC.
4.77 DHSC and NIHR could benefit from mutual learning with leading international funders of global health research. In stakeholder interviews, the Canadian International Development Research Centre (IDRC) was regularly cited as an example of good practice, with lessons to share on direct funding to LMIC institutions, gender, and equity.
Mechanisms to support ongoing cross-departmental learning on global health research vary in their effectiveness, and learning between departments tends to be ad hoc
4.78 When DHSC was first allocated ODA, the department engaged proactively with DFID to understand how to spend this money effectively. Some DFID staff transferred to DHSC, including at senior levels, which facilitated knowledge sharing. Civil service moves between FCDO and DHSC remain frequent in both directions. However, formal interdepartmental working group meetings, which were once held monthly, have now become ad hoc and less frequent. Departmental coordination depends on personal relationships and informal information sharing, particularly between DHSC’s GHR portfolio managers and the health team within FCDO Research and Evidence Directorate (RED). The Chief Scientific Advisers from FCDO and DHSC hold regular formal meetings that cover a range of topics, including research.
4.79 Other mechanisms for continued DHSC engagement with and learning from FCDO and other government departments include DHSC participation in the cross-government ODA oversight group and UKCDR funders’ groups, ongoing FCDO and DSIT observation of the GHR portfolio’s Independent Scientific Advisory Group (ISAG), and FCDO involvement in DHSC’s GHS programme board. There was also a one-off cross-government learning event on equitable partnerships for GHS. DHSC attempted to arrange a ‘teach-in’ with FCDO RED and Science and Innovation Network (SIN) representatives to share information about its ODA-funded research, but this never materialised.
4.80 When developing its own funding schemes, such as the GHR Groups and Units and the RIGHT programme, NIHR emphasised learning by doing rather than learning from and adapting approaches tested by the MRC, Wellcome, and DFID/FCDO, such as the effective use of logframes for research projects and the development of pathways to impact. In this respect, NIHR’s ODA learning curve was unnecessarily steep. More positively, NIHR recently engaged FCDO’s Evaluation Quality Assurance and Learning Service (EQuALS) to help refresh its programme-level theories of change. DHSC has also taken on board the findings from ICAI’s review of the Newton Fund when developing its GHR portfolio, which is reflected in NIHR’s ongoing efforts to increase ODA flows to LMIC research institutions.
There has been limited portfolio-level learning, particularly related to impact, but this is starting to improve
4.81 DHSC approaches to portfolio-level learning have been ad hoc with some significant gaps, particularly on learning related to impact. Overall, the department’s approach to portfolio-level learning is fragmented rather than deliberate and strategic.
4.82On GHR, NIHR has driven the learning agenda. DHSC told ICAI that the department lacks the resources to lead on this. For synthesis on cross-cutting topics such as equitable partnerships, capacity strengthening and impact, NIHR has relied heavily on UKCDR. However, UKCDR’s knowledge outputs are infrequent, broad and general, rather than specific to global health research. NIHR has drafted several impact case studies, as well as examples of equitable partnerships and capacity strengthening, but it has been slow to publish these. A wide range of global health research case studies has been made available via the NIHR website, but these are mostly project summaries or snapshots of activity in a particular area rather than learning tools. DHSC and NIHR are not doing enough to share learning from both the GHR and GHS portfolios on developing pathways to impact, including on failures as well as successes.
4.83 GHR portfolio-level learning is improving, aided by the recent GHR portfolio evaluation and by the new GHR programme director’s proactive engagement. DHSC and NIHR have plans to refresh the GHR portfolio-level theory of change, to conduct a deep dive review of CEI, and to review resourcing for learning. However, there is no GHS monitoring, evaluation and learning (MEL) strategy, nor is there a systematic approach to learning at GHS portfolio level.
4.84 Opportunities for cross-portfolio learning within DHSC, for instance on shared principles and challenges such as equitable partnerships and capacity strengthening, appear somewhat limited. DHSC holds ODA learning days across GHR and GHS, which are organised by a central programme management office. Other cross-portfolio fora are not focused specifically on learning, although DHSC does consider them to be learning mechanisms. Examples include the department’s ODA Policy Working Group and its ODA Transparency Working Group. GHR and GHS portfolio representatives also sit in on each other’s programme board meetings.
4.85 ICAI found that the completion of programme-level annual reviews has been inconsistent and publication via DevTracker has been slow, particularly across the GHR portfolio. Some aspects of the DHSC annual report format undermine its value for programme-level monitoring and evaluation. For example, the section on impact omits key activities that could foster impact, such as evidence synthesis and other knowledge translation activities.
4.86 As noted previously, the first evaluation of the GHR portfolio has recently concluded, and an evaluation of the JGHT programme was conducted in 2019. No GHS portfolio-level evaluation has yet been commissioned despite having been mooted in 2020. However, several independent evaluations have been undertaken for the GHS programmes assessed by ICAI, namely GAMRIF, UKVN and UK-PHRST. All GHS evaluations are published.
4.87 ICAI found good evidence that, where evaluations have been conducted, findings are being used to support learning and improvement. For example, the GAMRIF phase 1 evaluation findings and recommendations were used to shape phase 2 of the programme, and early UK-PHRST evaluations led to a strengthened approach to learning based on regular review and continuous improvement. The JGHT evaluation also kickstarted the development of a more robust approach to monitoring and learning across the programme.
Mechanisms for learning and adaptation within programmes have improved over the period, with LMIC researchers becoming more involved
After Action Reviews (AARs) are the preferred mechanism for learning and adaptation at programme level. Within the GHR portfolio, NIHR has completed 15 AARs to date and shared several examples of adaptations that were made to programmes and their governance as a result. However, only a small group of individuals at DHSC and NIHR is involved in these programme-level AARs, alongside a few UK delivery partners. ICAI saw no evidence of input from LMIC partners or experts. It is also not clear whether and how NIHR draws on feedback loops from project-level CEI to inform programme-level learning.
Some programmes have been designed to pilot new approaches and to enable iterative learning and adaptation, in particular the RIGHT programme (see Box 12). The GHR Centres scheme, which was developed more recently and has only run one call so far on non-communicable disease, is taking a different approach towards adaptive programming. NIHR has engaged an LMIC-led learning research partner to embed practices such as participatory MEL, action research, and continuous improvement across the programme and its various awards.
Box 12: Learning and adaptation in the RIGHT programme
The Research and Innovation for Global Health Transformation (RIGHT) programme offers a strong example of learning, adaptation and improvement, within the programme and across the wider GHR portfolio, as well as for NIHR institutionally. RIGHT is managed by the NIHR Central Commissioning Facility, which set up a new ODA team to run it, and as the first commissioned call within the NIHR global health research programme, its potential to pilot new approaches and generate useful learning was recognised by DHSC.
RIGHT introduced Proposal and Partnership Development Awards to foster relationship-building and the co-design of research projects between UK and LMIC researchers, in response to learning from the GHR Units and Groups, and this informed the Development Awards call that launched the Global HPSR programme. Through its piloting of approaches, RIGHT also had a formative influence on all NIHR ODAfunded programming in relation to the practice of community engagement and involvement (CEI). RIGHT built CEI into its awards from the outset, drawing on approaches used in UK health research. It was the first GHR programme to require applicants to include a CEI plan within their proposal, and every RIGHT funding panel has multiple dedicated CEI reviewers. The programme also introduced CEI workshops for shortlisted applicants to guide their proposal development, and it piloted an applicant webinar on impact strengthening, but this was not rolled out further.
The evolution of RIGHT shows clear progress on LMIC institutional engagement and leadership over time. For Call 1, UK applicants were only encouraged to engage LMIC partners in their projects, but for Call 2, an LMIC co-investigator or joint lead applicant was required. By Call 3, projects required joint leads in the UK and in an LMIC partner institution, but with the UK institution receiving and allocating funds. However, from Call 4 onwards, LMIC researchers have been able to apply in their own right, making RIGHT the first NIHR programme to directly fund LMIC institutions.
4.90 Within GHR programmes, there is significant potential for learning and sharing of good practice across projects, which is just starting to be realised. Early sessions bringing together cohorts of researchers supported through the same call were UK-focused and UK-dominated, but DHSC and NIHR are now facilitating shared learning between research projects supported by different programmes, offering good potential for networking within countries and for peer learning across countries. For example, DHSC and NIHR recently held roundtable events with researchers and stakeholders in four LMICs, and the NIHR GHR Academy’s training programme meetings bring together all the country-level training leads. The inaugural NIHR shared learning event in late 2023 also involved researchers from a range of different NIHR awards, but the GHR Groups and Units were dominant. Some LMIC-based researchers participated in this event, although none presented their projects or related learning.
Conclusion on learning
4.91 With an increased emphasis on learning and adaptation now evident, alongside some signs of improved engagement by LMIC researchers, DHSC is starting to share, scale up and adapt effective global health research practice across the GHR portfolio, if not yet across the GHS portfolio. The department is evidently keen to adapt and improve its ODA-funded programming, and it has used opportunities to pilot and innovate to good effect. In recognition of this, we award a green-amber score for learning.
5. Conclusions and recommendations
5.1 The UK spends a large share of its health official development assistance (ODA) on research, and much of this aid is now managed by the Department of Health and Social Care (DHSC). Since receiving its first ODA allocations, DHSC has supported research and innovation to improve global health security and to tackle antimicrobial resistance (AMR), and the UK has adopted a lead role on AMR internationally. The National Institute for Health and Care Research (NIHR) has also established itself as a major funder of global health research.
5.2 During the period under review, DHSC’s global health research portfolios have remained aligned with UK government strategy, which prioritises the development of the UK science base, global research and development (R&D) partnerships, and resilience to global health threats. Alongside this, the department has sought expert input and taken account of the wider funding landscape when developing new programmes or funding calls. However, input from low- and middle-income country (LMIC) stakeholders to DHSC’s strategic approach and priority-setting remains limited.
5.3 DHSC’s ODA-funded research portfolios are now maturing, and as more projects draw to a close, this area of substantial health ODA expenditure will rightly be subjected to greater scrutiny around its development impact and value for money. Some projects are already contributing to improved health outcomes, most obviously through the development of vaccines for typhoid and COVID-19. However, DHSC programming has not yet paid sufficient attention to research impact pathways, particularly those involving rigorous evidence synthesis. Coordination with Foreign, Commonwealth and Development Office (FCDO) in LMIC contexts, and in areas such as identifying opportunities for evidence translation, has been limited. DHSC does not have a deliberate approach to untying aid across all funding schemes, which hinders LMIC researchers’ ability to form partnerships that will maximise research quality and impact.
5.4 DHSC is attentive to ODA eligibility and takes ODA management seriously. The department makes innovative use of community engagement and involvement (CEI) to strengthen research projects and deliver localised benefits. It is committed to equitable partnerships and capacity strengthening, and strong results can be seen at the level of individual capacity strengthening, including large numbers of LMIC researchers benefitting from training programmes. However, the approach to capacity strengthening at the institutional or system levels is less considered, which reduces prospects for contributing to transformational change and greater LMIC leadership in global health research.
5.5 DHSC’s principles have not been fully embedded across all global health research activities. LMIC perspectives are missing in many monitoring, evaluation and learning activities, for example. The department does not have appropriate metrics to assess its contributions to institutional or system-level capacity strengthening, and the Global Health Security (GHS) portfolio, in particular, does not have sufficiently clear expectations around equitable partnerships and capacity strengthening.
5.6 These issues aside, overall, DHSC’s ODA-funded global health research programmes are focused on generating benefits for people in LMICs, and ICAI observed a range of well-designed and context-appropriate projects. Some have already yielded impressive results. There has also been a positive trajectory during the period under review on many of the challenges noted. The department has engaged well with UK and international stakeholders, taking a proactive approach to learning from other funders of global health research and applying this on an ongoing basis to adapt its own programming. DHSC’s relevant research portfolios, its conscientious approach to ODA management, and its continuing efforts to strengthen its ODA-funded research programming, together merit an overall green-amber score.
Recommendations
ICAI’s recommendations to DHSC seek to address the challenges highlighted above, while also complementing, rather than duplicating, the recommendations offered by the recent GHR portfolio-level evaluation.
Recommendation 1: DHSC should focus on pathways to impact across its global health research portfolios, including by strengthening guidance for potential applicants and putting in place mechanisms for planning and measuring impact.
Problem statements:
- DHSC’s monitoring and reporting of results to ensure accountability for research impact are weak, considering the scale of the department’s ODA expenditure on global health research.
- There has been limited learning from FCDO and international good practice on pathways to impact for research.
- Scant guidance is provided to DHSC or NIHR funding applicants or awardees on identifying and measuring research impact.
- Impact pathways are often not sufficiently developed or applied.
- The role of evidence synthesis as an impact pathway is overlooked.
- Many project- and programme-level results frameworks do not focus on impact.
- There have been few impact case studies published to date.
- Selection criteria for impact case studies are unclear.
Recommendation 2: DHSC should ensure that its principle of equitable partnership is embedded and tracked across all areas of activity related to its global health research portfolios, including research funding, knowledge translation, learning, programme monitoring and evaluation.
Problem statements:
- Until late 2020, NIHR was unable to provide direct funding to LMIC institutions.
- The onerous administrative and financial reporting requirements of NIHR awards risk putting off new or repeat LMIC applicants.
- Success rates for LMIC applicants to funding schemes are relatively low.
- Some UK-led awards show limited engagement by LMIC partners in research dissemination and evidence translation.
- The voices and perspectives of LMIC partners and experts have had limited profile and influence so far within DHSC and NIHR learning activities.
- The NIHR editorial team responsible for all NIHR journals, including the global health journal, currently has no LMIC members.
- The concept of equitable partnerships is not well defined for the GHS portfolio, and it is often conflated with aid untying.
- Qualitative data (specifically LMIC partner feedback) are not routinely gathered to assess progress towards equitable partnerships.
Recommendation 3: DHSC should progressively untie its aid for global health research, to ensure value for money and to allow low- and middle-income country researchers to identify the most appropriate partners for their projects.
Problem statements:
- Value for money is compromised when aid is tied to the UK.
- Research quality may suffer if funding restrictions bar institutions from freely choosing their collaborators based on expertise and best fit rather than geographical location.
- Early global health research programming required a UK institutional lead, as did the UK Vaccine Network until very recently.
- Even where projects are led by LMIC institutions, their ability to choose partners from high-income countries other than the UK has been limited.
- An overly UK-centric approach risks missing opportunities to leverage third-party support and access global partnerships.
Recommendation 4: DHSC should purposively collaborate with FCDO to strengthen UK health ODA coherence and alignment to partner country needs and priorities.
Problem statements:
- UK embassies and FCDO health advisers do not have access to accurate information about DHSC-funded research projects in partner countries.
- UK ODA programming on health appears fragmented to partners, including to LMIC health ministries.
- There is limited interaction between DHSC programming and FCDO’s programming or health and science advisory networks in LMICs.
- There is little strategic engagement with the research priorities and ambitions of LMIC governments.
Recommendation 5: DHSC and NIHR should take a more strategic approach towards institutional and system-level research capacity strengthening in low- and middle-income countries, and develop metrics to track plausible contributions in these areas.
Problem statements:
- DHSC ambitions regarding LMIC research capacity strengthening are not clear.
- The current approach is strongly focused on individuals, despite a stated intent to strengthen institutional and system-level capacity.
- The potential of CEI to contribute to system-level capacity strengthening has not been considered.
- DHSC’s significant ODA health research spend is currently thinly spread.
Annex 1: Sampled programmes
| Name | Brief description | Indicative financial commitment | Actual start date | Planned end date | Review component | Spend (actual and projected) in review period |
|---|---|---|---|---|---|---|
| GHR – NIHR core and capacity-building programming | ||||||
| 1. NIHR Global Health Research Groups | The NIHR Global Health Research Groups programme funds research to address locally identified challenges in LMICs, by supporting equitable research partnerships between researchers and institutions in LMICs and the UK. It aims to generate evidence for improved health outcomes and build sustainable research capacity in LMICs. Funding of up to £3m over 4 years is available to research groups either new to delivering applied health research globally or wishing to expand an existing partnership. To date, 70 Groups have been funded across three calls. | Up to £175.65m | 01/06/2017 | 31/08/2026 | • Strategic review • Programme review • Malawi case study • India case study | £145.93m |
| 2. NIHR Global Health Research Units | The NIHR Global Health Research Units programme funds ambitious collaborative research projects to address locally identified challenges in LMICs, by supporting equitable partnerships between universities and research institutes in LMICs and the UK. It aims to generate evidence for improved health outcomes and strengthen research capabilities in LMICs. Funding of up to £7m over 5 years is awarded to partnerships with established track records in delivering internationally recognised global health research. To date, 23 Units have been funded across two calls. | Up to £153.87m | 01/06/2017 | 31/08/2027 | • Strategic review • Programme review • Malawi case study • India case study • Brazil case study | £103.63m |
| 3. NIHR Research and Innovation for Global Health Transformation (RIGHT) | The NIHR RIGHT programme funds interdisciplinary applied health research in LMICs on areas of unmet need where a strategic and targeted injection of funds can result in a transformative impact. It prioritises research benefitting LMIC populations while fostering capacity building and knowledge exchange through equitable partnerships in LMICs and between LMIC and UK researchers, and by promoting interdisciplinary collaboration. Each call has a focus on a different thematic priority and funds awards between £1m and £5m over up to 5 years. To date, 31 RIGHT awards have been made across five calls. | Up to £113.53m | 01/09/2019 | 31/12/2028 | • Strategic review • Programme review • Malawi case study • India case study • Brazil case study • Citizen engagement | £73.09m |
| 4. NIHR Global Health Policy and Systems Research (Global HPSR) | The NIHR Global HPSR programme funds health policy and systems research that is directly and primarily of benefit to people in LMICs, by supporting equitable partnerships in LMICs and between LMICs and the UK. It aims to generate evidence to improve health systems and inform policy and practice in LMICs, which will lead to improved outcomes for the most vulnerable and address issues of health equity. Phase 1 of the programme comprised three calls and funded 17 Global HPSR Development Awards (up to £0.1m over 15 months), 5 Commissioned Awards (between £1m and £4m over 4 years) and 8 Researcher-led Awards (between £1m and £4m over 4 years). | Up to £44.43m | 01/03/2020 | 30/11/2026 | • Strategic review • Programme review • Malawi case study • India case study • Brazil case study | £32.09m |
| 5. NIHR Global Research Professorships | The NIHR Global Research Professorships programme funds research leaders with a track record of applied health research in LMICs, to promote effective translation of research and to strengthen research leadership at the highest academic levels. Funding of up to £2m over up to 5 years is awarded to Professorships working in close partnership with research institutions in LMICs. To date, 15 Global Research Professorships have been funded across six calls. | Up to £28.98m | 01/11/2018 | 28/02/2029 | • Strategic review • Programme review • Malawi case study • India case study | £18.65m |
| GHR – NIHR partnership programming | ||||||
| 6. NIHR-Wellcome Global Health Research Partnership – Wellcome | The NIHR-Wellcome Global Health Research Partnership funded existing work developed by Wellcome to support postgraduate students and postdoctoral and early-career researchers from LMICs and the UK, with a focus on research in health priority areas for LMICs and activities to improve research uptake into policy. | Up to £29.34m | 18/04/2019 | 31/03/2028 | • Strategic review • Programme review • Malawi case study • India case study • Brazil case study | £16.96m |
| 7. Global Effort on COVID-19 (GECO) Health Research – MRC | GECO was a rapid UK cross-government funding call aiming to support applied health research that would address COVID-19 knowledge gaps in ODA-eligible countries, aligned to the WHO COVID-19 research roadmap. | Up to £10.00m | 02/09/2020 | 30/09/2023 | • Strategic review • Programme review • Malawi case study • India case study | £8.07m |
| 8. Joint Global Health Trials Initiative (JGHT) – MRC | JGHT is a UK cross-government initiative aiming to generate new knowledge to contribute to improving health in LMICs. It focuses on late-stage clinical research and smaller pilot studies that yield implementable results and address the major causes of mortality or morbidity in LMICs. | Up to £50.45m | 07/12/2016 | 31/3/2027 | • Strategic review • Programme review • India case study | £30.40m |
| 9. Royal Society of Tropical Medicine and Hygiene (RSTMH) Small Grants/Early Career Grants Scheme – RSTMH | The RSTMH Early Career Grants Scheme supports LMIC-based early-career researchers to develop their research skills and expertise. This partnership contributes to the NIHR Global Health Research priority to strengthen research capacity in LMICs. | Up to £6.64m | 16/07/2019 | 30/09/2027 | • Strategic review • Programme review • Malawi case study • India case study | £4.94m |
| 10. Global Mental Health programme – Grand Challenges Canada (GCC) | The Global Mental Health programme supports high-impact innovations that improve treatments and expand access to care for people living with or at risk of mental health disorders, with a focus on the mental health needs of young people in LMICs. | Up to £6m | 01/10/2019 | 31/03/2024 | • Strategic review • Programme review | £6m |
| GHS - Global Health Security research and innovation programmes | ||||||
| 11. UK Public Health Rapid Support Team (UK-PHRST) – research component | The research component of UK-PHRST collaborates with partners to conduct research to develop the evidence base for best practice in epidemic preparedness and response in ODA-eligible countries, and to develop local research capacity. | Up to £16.66m | 01/04/2016 | 31/03/2025 | • Strategic review • Programme review • Malawi case study | £13.90m |
| 12. Global AMR Innovation Fund (GAMRIF) | GAMRIF is a UK aid fund that supports research and development around the world to reduce the threat of antimicrobial resistance in humans, animals, and the environment, for the benefit of people in LMICs. | Up to £131.65m | 01/01/2017 | 31/03/2027 | • Strategic review • Programme review • Malawi case study • India case study | £114.14m |
| 13. UK Vaccine Network (UKVN) | UKVN targets funds to support the development of new vaccines and vaccine technologies for emerging infectious disease threats in LMICs, to support better control in the future of disease outbreaks that risk becoming epidemics. | Up to £198.45m | 01/02/2016 | 31/03/2028 | • Strategic review • Programme review | £137.08m |