The UK Department of Health and Social Care’s aid-funded global health research and innovation
1. Purpose, scope and rationale
Global health research aims to advance knowledge and innovation to improve health outcomes and achieve health equity globally, with a particular focus on the needs and priorities of low- and middle-income countries (LMICs). This area of research grew significantly in scale and importance globally during the COVID-19 pandemic, and it has become more central to the strategic priorities of the UK international development programme. Aid-funded global health research is also central to the UK’s contribution to achieving the Sustainable Development Goals (SDGs) (see Box 1).
This will be the first ICAI review focused specifically on global health research and the first to focus solely on aid spending by the UK Department of Health and Social Care (DHSC), which until now has not been covered as extensively as other government departments that spend significant amounts of official development assistance (ODA). The review will add value by shining a light on an area of aid expenditure that has received little attention from scrutiny bodies.
The review is an opportunity to revisit and build on previous ICAI reviews, including the 2018 review of the UK’s response to global health threats and research-focused reviews such as those of the Global Challenges Research Fund (GCRF) and the Newton Fund. It is also relevant to ICAI’s COVID-19 reviews, although these did not specifically focus on research and innovation funded through DHSC. ICAI’s 2023 synthesis review mentions global health research and notes that DHSC awards to Oxford University through the UK Vaccine Network from 2016 onwards laid important foundations for, and subsequently supported, the development of the Oxford-AstraZeneca COVID-19 vaccine.
Box 1: Global health research and the SDGs
Funding of global health research contributes towards both SDG 3 and SDG 9.
![]() SDG 3: Ensure healthy lives and promote well-being for all at all ages.
SDG 3: Ensure healthy lives and promote well-being for all at all ages.
- Target 3.b: “Support the research and development of vaccines and medicines for the communicable and non-communicable diseases that primarily affect developing countries…”
![]() SDG 9: Build resilient infrastructure, promote inclusive and sustainable industrialisation and foster innovation.
SDG 9: Build resilient infrastructure, promote inclusive and sustainable industrialisation and foster innovation.
- Target 9.5: “Enhance scientific research, upgrade the technological capabilities of industrial sectors in all countries, in particular developing countries, including, by 2030, encouraging innovation and substantially increasing the number of research and development workers per 1 million people and public and private research and development spending.”
- Target 9.b: “Support domestic technology development, research and innovation in developing countries…”
2. Background
Global health is a broad and multidisciplinary field aimed at “improving health and achieving equity in health for all people worldwide”. Research in this area emphasises transnational health issues and promotes collaboration between basic and applied science, biomedical and clinical research, health policy and management, public health and epidemiological studies, and health-related environmental, economic and social research.
The World Health Organisation (WHO) sits at the centre of the global health architecture. Among its functions is the promotion and conduct of global health research. Since 1975, WHO has co-sponsored a Special Programme for Research and Training in Tropical Diseases (TDR), which aims to support global health research, strengthen research capacity in “disease-affected countries” and translate evidence into practice to reduce infectious disease and build resilience in the most vulnerable populations. However, despite substantial support for global health research, a “stark contrast between the global distribution of sickness and death, and the allocation of health research funding” persisted into the 1990s, with less than 10% of health research spending devoted to 90% of the global disease burden (known as the 10/90 gap). The past two decades have witnessed a proliferation of public-private partnerships and other global health research initiatives designed to close this gap.
The UK has played a significant role in many of these global health research initiatives and partnerships. Its engagement in global health research dates back to the establishment of ‘tropical medicine’ centres in the late 19th century. More recently, the UK has allocated ODA to global health research. Until the 2014-16 Ebola epidemic in West Africa, which intensified global health security concerns across the UK government, ODA for global health research had been allocated by the former Department for International Development (DFID). DHSC received its first ODA allocations for research through the 2015 spending review. The 2015 UK Aid Strategy referenced several new health research initiatives, including the UK Vaccine Network and the Global Antimicrobial Resistance (AMR) Innovation Fund (GAMRIF). Support to vaccine research and innovation was further enhanced in response to the COVID-19 pandemic.
As illustrated by Figure 1, which shows DHSC’s actual and forecast ODA expenditure on global health research from 2018-19 onwards, aid funding supports two different strands of programming. The global health research strand encompasses several large funding schemes managed by the National Institute for Health and Care Research (NIHR). It also covers NIHR partnership programmes run by other UK or international organisations such as the European and Developing Countries Clinical Trials Partnership (EDCTP), WHO, the World Bank, Wellcome and the Medical Research Council (MRC). The global health security strand includes two DHSC research programmes and one programme with a research component, which work through external delivery partners. The department also contributes ODA to the Coalition for Epidemic Preparedness Innovations (CEPI), which is shown separately in Figure 1.
There was a rise in UK ODA funding for global health research in the years following the West African Ebola epidemic in 2014-16. Figure 1, showing DHSC expenditure from financial year 2018-19 (actual) to 2024-25 (projected), indicates a growing budget until 2019-20. Then, as the UK reduced its ODA spending from 0.7% to 0.5% of gross national income (GNI) in 2020-21, aid for global health research dropped significantly, while funding for research on global health security (including CEPI) flatlined. The DHSC ODA budget for research increased again after the onset of the COVID-19 pandemic, even when the overall UK ODA budget was effectively cut by 29%, as it was diverted to support asylum seekers and refugees in the UK.
Figure 1: DHSC ODA expenditure on global health research 2018-19 to 2024-25
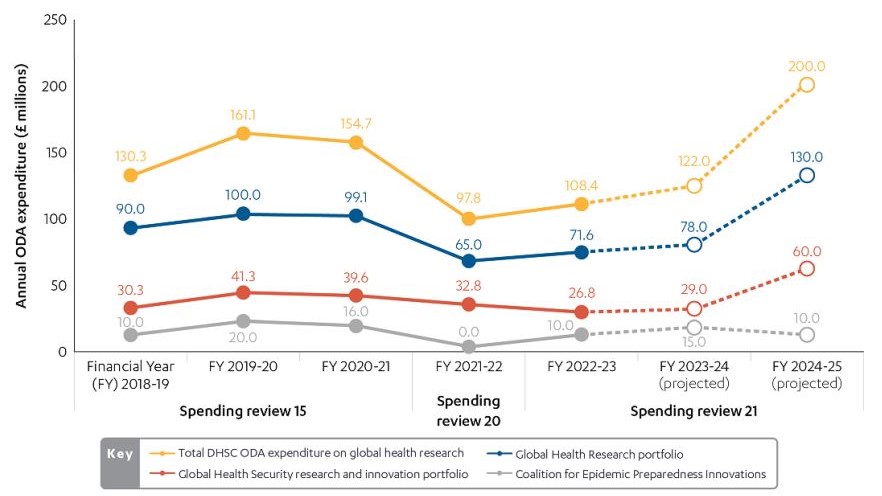
Figure 1 shows actual spend by UK financial year for 2018-2019 to 2022-2023 and projected expenditure for 2023-2024. Projections are indicative and future expenditure may be affected by changing global needs, including humanitarian crises, fluctuations in GNI and other ODA allocation decisions.
In the time period covered by this review, the Foreign, Commonwealth and Development Office (FCDO) and the Department for Science, Innovation and Technology (DSIT) have also spent ODA to support health-related research and innovation. Since ICAI’s GCRF review, which found that better cross-government coordination of ODA-funded research was urgently needed, the use of UK ODA for research has been coordinated by the Strategic Coherence of ODA-funded Research (SCOR) Board managed by the UK Collaborative on Development Research (UKCDR). UKCDR also serves as secretariat to the Health Funders Forum (HFF), which has operated since 2007 and meets three times a year to support coherence across UK funding to global health research.19 DHSC is a member alongside FCDO, UK Research and Innovation (UKRI), the MRC and several other research councils, the Academy of Medical Sciences (AMS), and Wellcome.
The UK’s global health research is strongly focused on global health security and on furthering the UK’s role internationally as a leader in science and technology (see Box 2). However, to be ODA-eligible, research must be conducted for the primary benefit of low- and middle-income countries, in line with the rules established by the Development Assistance Committee of the Organisation for Economic Cooperation and Development (OECD-DAC). Benefits that align with OECD-DAC definitions include public health or social welfare (for example, if research is focused on diseases or health issues that primarily affect people in ODA-eligible countries) and economic benefits (for example, where research is undertaken by institutions in ODA-eligible countries). Benefits to low- and middle-income countries also take the form of health research capacity development, such as training, the sharing of knowledge and intellectual property, and the transfer of technologies.
Box 2: Current UK strategy and global health research
Several recent UK government publications outline the high-level strategic framework for DHSC’s ongoing support to global health research.
Integrated Review (2021): This confirms the Spending Review 2020 allocation of £1.3 billion to DHSC for research and innovation to support “health resilience”. It commits to accelerating the development and deployment of vaccines, therapeutics and diagnostics for “emerging diseases”. Global health security and science and technology are cited as ODA priorities for 2021-22.
Strategy for International Development (2022): This strategy states that the UK will “invest in the research and innovations needed to keep driving breakthroughs in health systems and health security… to respond to the changing burden of disease and health threats, including from COVID-19, antimicrobial resistance (AMR) and zoonoses”.
White Paper on International Development (2023): Chapter 8 of this white paper, which covers research, innovation and new technologies, includes health among key priorities. It calls for a “collective global mobilisation of scientific expertise, research and innovation” for the SDGs, including to achieve “breakthroughs in and ensuring access to affordable life-saving health technologies”. The white paper emphasises science and research partnerships that are “led, by and with, low- and middle-income countries, and that focus on mutually agreed priorities”.
Global Health Framework (2023-25): This framework, the implementation of which is jointly led by FCDO and DHSC, includes an objective to “advance UK leadership in science and technology, strengthening the global health research base of UK and partner countries, while supporting trade and investment”.
Even where global health research is of clear primary benefit to ODA-eligible countries, there may be significant barriers to research uptake. For example, some health systems may lack the resources to deploy updated guidelines or new health technologies. This demonstrates the value of ODA funding for research that can inform health policy, financing and system strengthening, as well as public health interventions and technologies.
This review will cover the full breadth of global health research funded by DHSC. In addition to research targeting specific global health challenges such as AMR, this includes global health security programmes with a research component, innovation programmes focused on new vaccines and other health technologies, research programmes focused on health policy and systems, and initiatives to strengthen research capacity in low- and middle-income countries.
3. Review questions
The review is built around the evaluation criteria of relevance, effectiveness and learning, addressing the questions and sub-questions in Table 1.
Table 1: Our review questions
| Review criteria and questions | Sub-questions |
|---|---|
| Relevance: How relevant is DHSC’s ODA-funded global health research portfolio to the UK’s strategic objectives on global health? | •Does DHSC have a credible strategy for directing health research to meet global health needs and priorities? •How appropriate is DHSC’s approach to building equitable research partnerships? •How effectively does DHSC screen and monitor its research grants for ODA eligibility and for consistency with UK commitments on tied aid? |
| Effectiveness: How effectively does DHSC’s ODA-funded research contribute to improving global health outcomes? | •How well has DHSC-funded global health research contributed to improvements in health practice in low- and middle-income countries? •How well have DHSC-funded research programmes disseminated their results and supported other pathways to impact? •How well has DHSC enhanced research capacity in low- and middle-income countries? |
| Learning: Has the design of DHSC’s research portfolio been informed by its own monitoring, evaluation and learning, and by lessons from other ODA-funded health research? | •How well has DHSC learned from other ODA programmes that aim to carry out research or to build research and innovation capacity? • How well do DHSC managers of global health research programmes and their implementers adapt in response to lessons learned? |
4. Methodology
The methodology for this review has been designed around five components that will enable us to address our review questions and ensure sufficient triangulation of the evidence within the four-month window for data gathering and analysis (see Figure 2).
Figure 2: Our methodology
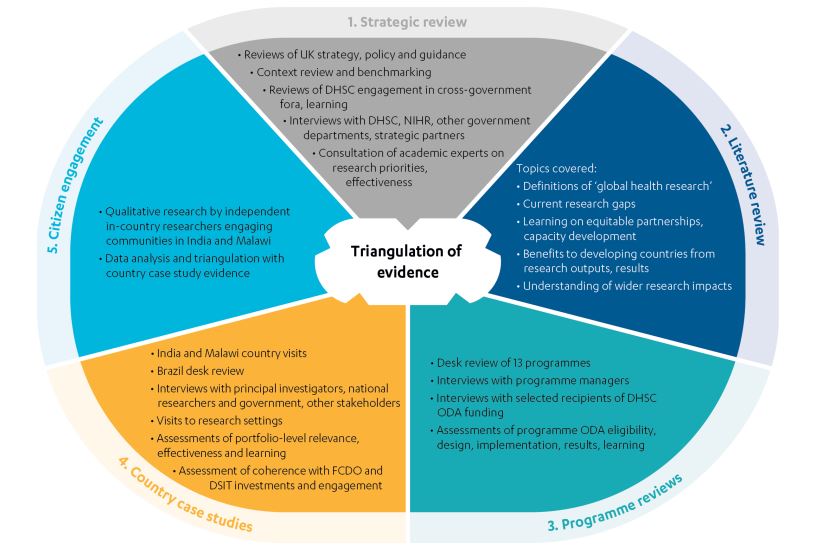
Component 1 – Strategic review: To address our review question on relevance, the strategic review covers DHSC strategies, policies and guidance related to research prioritisation, funding and oversight. It also includes the UK government’s wider strategies on global health, science, and innovation, alongside WHO and OECD-DAC guidance on ODA and research that the UK is expected to follow. To address our review question on learning, the strategic review examines DHSC engagement in cross-government research fora and participation in other learning opportunities. The document review is complemented by interviews with senior officials at DHSC, FCDO and DSIT, and with representatives of NIHR and DHSC’s strategic partners. In addition to government sources, the strategic review also builds on perspectives on current priorities and good practice provided by independent academic experts and other UK and international funders of global health research
Component 2 – Literature review: The literature review covers a selection of available peer-reviewed literature on global health research alongside key grey literature. It examines how ‘global health research’ is defined and how its impact is understood and assessed. It also identifies current research gaps, documents learning about equitable partnerships and capacity development, and assesses the evidence on how LMICs benefit from health research capacity, outputs and results. The literature review contextualises DHSC’s efforts to build equitable research partnerships and to strengthen health research capacity in LMICs. It provides a frame of reference for the strategic and programme reviews, enabling us to assess DHSC’s approach in relation to the broader evidence base.
Component 3 – Programme reviews: These consist of desk reviews of a sample of 13 programmes, examining relevant documents and conducting interviews with programme managers in DHSC, NIHR and relevant partner organisations, as well as with selected research institutions in receipt of DHSC ODA. We have identified a sample of programmes based on the criteria described in Section 5 below. The programme reviews focus on whether programme designs are evidence-based and consistent with rules on ODA eligibility and commitments to untied aid. They also assess the extent to which programmes are implemented effectively and achieving their intended results, and the degree to which learning leads to adaptation and improvement.
Component 4 – Country case studies: We conducted two country visits to India and Malawi and one country desk review of Brazil. The case studies assessed the DHSC global health research portfolio in each country, collecting and analysing evidence on the relevance and effectiveness of DHSC-funded research projects, and the extent to which learning from different country contexts was documented and applied by DHSC. We examined the contribution of DHSC-funded projects within the context of wider UK ODA flows to the research sector in India and Malawi and assessed how DHSC programming linked up with FCDO health sector engagement and DSIT funding for the science base. The case studies triangulated research project reporting and outputs with evidence from interviews with principal investigators and other researchers, national government and other stakeholders, as well as with feedback from people expected to benefit from UK aid (Component 5).
Component 5 – Citizen engagement (with people affected by or expected to benefit from UK aid): ICAI is committed to incorporating the voice of people affected by UK aid into its reviews. Qualitative research in India and Malawi is undertaken by national research partners. Their consultations include people who are expected to benefit from research outputs such as new health products or technologies. The findings from this engagement contribute to the assessment of whether DHSC-funded research is relevant to people’s needs, whether it addresses their priorities effectively, and whether any potential risks or unintended consequences are assessed and mitigated. It also contributes to the assessment of how DHSC ODA-funded research engages with communities, drawing on evidence from a small sample of projects.
5. Sampling approach
The methodology involves two areas of sampling: the selection of programmes for desk review, and the selection of case study countries. The two samples were cross-referenced to ensure that the country visits covered a representative sample of activities falling under the 13 programmes we selected for desk review.
For the programme desk reviews, our sample was selected from the 24 ODA-funded programmes within DHSC’s global health research portfolio. We used purposive sampling based on five criteria (programme type, relevance, status, budget, and presence in case study countries) as shown in Table 2.
Table 2: Sampling criteria applied for this review
| Sampling criteria | Categories |
|---|---|
| Programme type | •NIHR-managed global health research programme •NIHR partnership programme • Global health security programme with research focus/component |
| Programme relevance | • Core programme • Supplementary or complementary programme |
| Programme status | • Active • Closed |
| Projected programme spend | • Small (£0-10 million) •Medium (£10-50 million) • Large (£50 million+) |
| Country presence | •India •Malawi •Brazil |
We then selected 13 programmes as offering a representative sample across all criteria. These are listed in Table 3. The programmes selected represent approximately 73% of the actual and projected DHSC ODA spend on global health research during the period from 2018-19 to 2024-25.
Table 3: Programmes sampled for desk review
| Type | Programmes | Spend (actual and projected) in review period |
|---|---|---|
| NIHR-managed programmes | •NIHR Global Health Research Groups 30 •NIHR Global Health Research Units 31 •NIHR Research and Innovation for Global Health Transformation (RIGHT) •NIHR Global Health Policy and Systems Research (Global HPSR) •NIHR Global Research Professorships | • £144.76m • £103.00m • £75.71m • £31.28m • £19.17m |
| Global health security research and innovation programmes | • UK Public Health Rapid Support Team (UK-PHRST) – research component • Global AMR Innovation Fund (GAMRIF) • UK Vaccine Network (UKVN) | • £13.60m • £136.69m • £109.53m |
| NIHR partnership programmes | •NIHR-Wellcome Partnership on Global Health Research – Wellcome • Global Effort on COVID-19 Research (GECO) – MRC •Joint Global Health Trials Initiative (JGHT) – MRC • Royal Society of Tropical Medicine and Hygiene (RSTMH) Small Grants/Early Career Grants Scheme – RSTMH • Global Mental Health Programme – Grand Challenges Canada (GCC) | • £16.90m • £8.10m • £30.90m • £4.90m • £15.10m |
To select the country case studies, we first used UKCDR’s Mapping ODA Research and Innovation (MODARI) database, which identified 46 countries with at least one project supported by ODA funding from DHSC. Analysis of these data generated a longlist of 12 countries with a significant level of programming. These countries were further assessed to identify a representative sample across key criteria including diversity of programming, geographic region, and human and economic development indices. We also considered whether there were any projects led by national institutions or researchers, and whether it would be possible to identify communities and vulnerable groups which could potentially benefit from DHSC-funded research and could be reached through citizen engagement. Following discussion with DHSC and consideration of additional information provided by the department, we selected three countries based on these criteria, as summarised in Table 4.
Table 4: Country case studies sampled for visits or desk review
| Country | Programme representation | Other criteria |
|---|---|---|
| Malawi (visit) | •NIHR core and capacity-building programming •NIHR-Wellcome Partnership on Global Health Research • Global Effort on COVID-19 Research (GECO) – MRC •Joint Global Health Trials Initiative (JGHT) – MRC • Global AMR Innovation Fund (GAMRIF) • UK Public Health Rapid Support Team (UK-PHRST) – research component • Royal Society of Tropical Medicine and Hygiene (RSTMH) Small Grants/Early Career Grants Scheme – RSTMH | • Least developed country • Low-income country • Africa region •Not a member of UK Science and Innovation Network (SIN) |
| India (visit) | •NIHR core programming •Joint Global Health Trials Initiative (JGHT) – MRC • Global AMR Innovation Fund (GAMRIF) • Royal Society of Tropical Medicine and Hygiene (RSTMH) Small Grants/Early Career Grants Scheme – RSTMH | • Lower-middle income country • Asia region •Member of UK SIN |
| Brazil (desk review) | •NIHR core programming •NIHR-Wellcome Partnership on Global Health Research • UK Public Health Rapid Support Team (UK-PHRST) – research component • Royal Society of Tropical Medicine and Hygiene (RSTMH) Small Grants/Early Career Grants Scheme – RSTMH | • Upper-middle income country • South America region • Member of UK SIN |
The result is a sample that covers programming across both core strands of DHSC ODA allocation to research, namely global health research and global health security research and innovation. The global health research sample includes NIHR-managed funding schemes, as well as NIHR partnership programmes led by other UK institutions. This breadth of programming is well represented in our three case study countries, which are economically and geographically diverse. This will enable us to assess the contribution made by DHSC-funded research across a wide range of country contexts.
6. Limitations to the methodology
We anticipate three primary methodological challenges:
- Pathways to impact: Global health research and innovation funding may take many years to impact health and development outcomes. While some research projects focus on developing and piloting specific health interventions or technologies, where the potential for impact can be assessed in real time, other projects aim to build an evidence base that may (directly or indirectly) influence the development of health practice over a longer period. Furthermore, most of the sampled programmes are ongoing, and so many of the individual research projects are not yet completed. We therefore anticipate accessing limited results data across our sampled programmes. In mitigation, we examine research approaches, interim data, and progress reporting, alongside plans for the dissemination of research outputs, in order to assess the plausibility of envisaged pathways to development impact (and the implications for ODA eligibility).
- Generalisability of findings: The NIHR-managed research programmes, particularly the major funding schemes, are large and complex. Many UK-based academic and research institutions are funded through them, and each grantee partners with LMIC researchers and other organisations in the UK and across the world to undertake their research. We have identified a representative sample of such organisations in India and Malawi, but this accounts for a relatively small share of the whole, given the significant volume of research funded in this way through DHSC ODA. In mitigation, we triangulate our country case studies carefully with other evidence gathered through the review, in order to generate findings, noting where these are likely to be generalisable as opposed to context-specific.
- Short timescale: This review has a shorter timeline that would normally be the case for a full ICAI review, which means that different components of the methodology have had to run in parallel. To ensure that the different methodological components complemented and informed one another, the team took stock of interim insights across all components at key points during the evidence gathering phase. This will also help to ensure that the resulting findings are appropriately triangulated.
7. Risk management
This section covers external risks – factors beyond our control that might affect delivery – rather than methodological constraints, which are addressed under ‘limitations’. Most of the risks associated with this review arise from the tight timeline for its completion. Therefore, our mitigation strategies are focused on team and task management.
| Risks | Mitigation and management actions |
|---|---|
| Tight turnaround time for deliverables | ICAI has developed a strong implementation plan, and is monitoring its execution regularly and acting early to mitigate the impact of any delays. An early launch of the literature review and the identification of best practice in ODA-funded research, along with insights provided by expert team members, enabled the team to be sufficiently briefed prior to data collection. |
| Timeliness of engagement by DHSC with ICAI | ICAI has communicated clearly and regularly with DHSC colleagues about the shortened timeline and has set out expectations on response times and agreed on engagement points to ensure that the timeline can be upheld. |
| Short window to implement citizen engagement in two countries | This risk is addressed through early engagement, and co-creation of the citizen engagement approach, with the in-country research institutions, which are trusted partners that have worked with ICAI on previous occasions. |
| The relatively limited field of global health research creates challenges with finding experts and peer reviewers who do not have conflicts of interest due to other work funded through DHSC or NIHR | The team for this review draws on a larger than usual number of experts, in order to minimise individual experts commenting on or working in areas where they may have a conflict of interest. An extensive search was conducted to find an appropriate peer reviewer. |
8. Quality assurance
The review is being carried out under the guidance of ICAI Lead Commissioner Dr Tamsyn Barton, with support from the ICAI secretariat. The review is subject to quality assurance by the service provider consortium.
Both the methodology and the final report will be peer-reviewed by Dr Andrew Lee, an expert in global health and health security. Dr Lee is professor of public health at the University of Sheffield’s School of Medicine and Population Health, and a regional deputy director and consultant in global health with the UK Health Security Agency.
9. Timing and deliverables
The review is taking place over a ten-month period starting from September 2023.
| Phase | Timing and deliverables |
|---|---|
| Inception | Design phase: September – November 2023 Approach paper publication: February 2024 |
| Evidence gathering | Country visits: November – December 2023 Evidence pack: January 2024 Emerging findings presentation: February 2024 |
| Reporting | Report drafting: February – May 2024 Final report: June 2024 |