The UK’s work with the Global Fund
Introduction
The Global Fund to Fight AIDS, Tuberculosis and Malaria is the world’s largest funder of efforts to defeat three of the deadliest diseases affecting the world’s population. The Global Fund’s mission is to end these epidemics by 2030 in line with Sustainable Development Goal 3.3.
Box 1: Sustainable Development Goal 3.3
![]()
Sustainable Development Goal 3.3 aims to: “By 2030, end the epidemics of AIDS, tuberculosis, malaria and neglected tropical diseases and combat hepatitis, water-borne diseases and other communicable diseases.”
Founded in 2002, the Global Fund has invested more than $55 billion in over 100 low-income and middle-income countries during the past 20 years. It provides 30% of all international funding for HIV and AIDS programming, 63% for malaria and as much as 76% for tuberculosis. The UK has been the third-largest donor to the Global Fund over its lifetime and made the second-largest pledges in the last two replenishments.
This information note is written in the context of the Global Fund’s next round of fundraising, referred to as the seventh replenishment, which takes place in September 2022. The information note provides a factual account of the UK’s financial and strategic engagement with the Global Fund since 2019 and how this engagement fits into the UK’s development cooperation on health. It is not evaluative but concludes with a set of key questions for any future investigation by ICAI or other scrutiny bodies. The note draws on information provided by, and interviews with, officials in the Foreign, Commonwealth and Development Office (FCDO). We also reviewed documentary sources, interviewed Global Fund staff and consulted a range of UK civil society organisations and other stakeholders working with the Global Fund. We undertook two mini-case studies of Kenya and Nigeria, involving a document review and interviews with FCDO health advisers based in the two countries.
How does the Global Fund work?
The Global Fund is a financing mechanism and does not implement programmes directly. It is part of an international partnership with governments, civil society, the private sector and communities affected by the three diseases. About half of Global Fund resources are spent on commodities and its purchasing power and market-shaping work have achieved significant cost reductions on mosquito nets, drugs and other products. The board overseeing the Global Fund’s activities is unique in its composition, with its group of over 20 members drawn from donor and recipient countries, the private sector, civil society and affected communities. The UK has its own seat on the board, reflecting the scale of its financial contributions to the Global Fund.
Once donor funds have been pledged through replenishment exercises, the Global Fund allocates money to countries based on their burden of disease and income levels. Funding requests – primarily disease-specific, but also for more general health systems strengthening – are then developed within the recipient countries. The Global Fund has country teams based in Geneva, but no in-country presence, which helps it to maintain low operating costs. It provides grants to fund the country-based mechanisms necessary for the delivery of programmes, which are also supported by a range of other organisations. Known as Country Coordinating Mechanisms (CCMs), these are dedicated groups in each recipient country that have been set up specifically to work with the Global Fund. They are often led by national governments but also include groups affected by the three diseases, civil society organisations, the private sector and donors, with external technical support. The CCM model is a unique feature of the Global Fund.
The CCMs submit proposals to the Global Fund for assessment by an independent Technical Review Panel. This process aims to ensure that quality is maintained. Grants are approved by the Global Fund board before disbursement and then implemented by organisations known as ‘principal recipients’ and ‘sub-recipients’. These can be government agencies, multilateral organisations, civil society organisations or private companies, overseen by that country’s CCM. The Global Fund monitors progress and has a strong focus on outcome indicators for the three diseases, advised by an independent Technical Evaluation Reference Group (TERG) that reports to the board’s strategy committee. It also has an independent assurance function, the Office of the Inspector General, which audits progress and assesses the financial integrity of the Global Fund’s operations, including fraud and fiduciary risks. In our interviews with UK government staff, they stated that the Global Fund’s audit and investigations functions are strong.
Figure 1: Global Fund allocation of funding per disease from 2017-19 to 2020-22
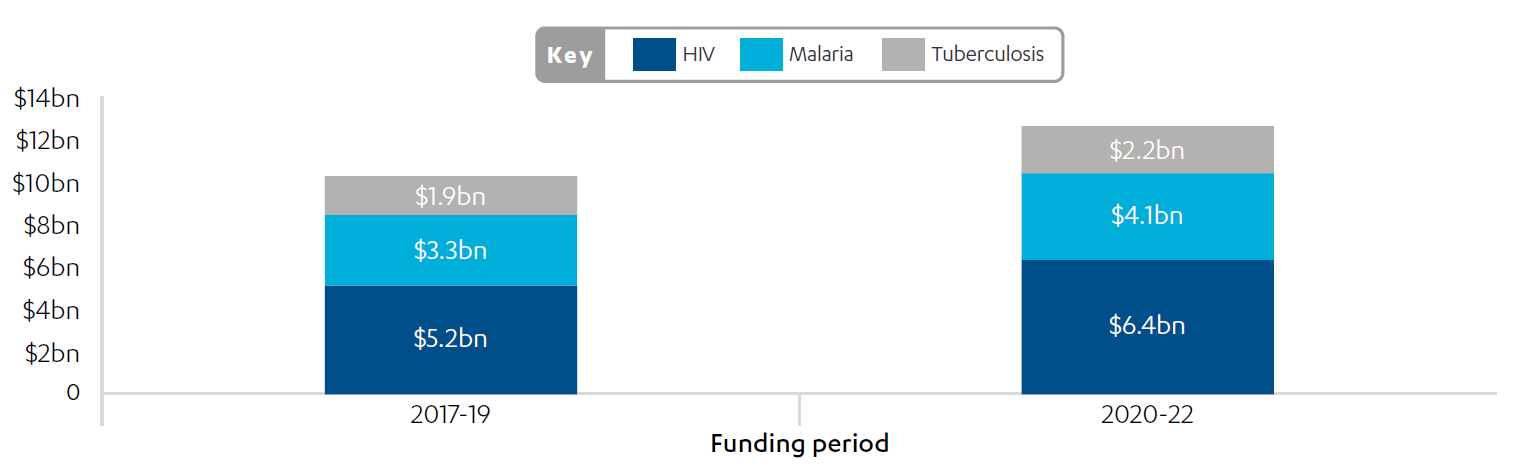
Source: The Global Fund data explorer, The Global Fund, accessed 7 July 2022.
The balance of Global Fund expenditure across the three diseases is a subject of lively debate and influenced by organisations representing those affected, with the strongest networks acting for people living with HIV and AIDS. The Global Fund recognises the need to do more on tuberculosis, which the UK supports. From January 2021 the Global Fund increased tuberculosis grants by 24% on average and committed the partnership to deploying more than $2 billion to fight the disease over the next three years. The Global Fund’s investment case for the seventh replenishment notes that the largest increase in projected funding needs in Global Fund countries is for tuberculosis care.
Box 2: Kenya case study
Kenya has been a Global Fund partner since 2003, with $782.3 million invested by July 2022 in HIV and AIDS programming, $390.7 million for malaria and $181.8 million for tuberculosis. Progress on HIV and AIDS is particularly striking, with AIDS-related deaths down 84% and new HIV infections down 69% since 2002. The number of new HIV infections among adolescent girls and young women has fallen by 50% since 2010. However, HIV testing numbers fell during the COVID-19 pandemic, with four million fewer people tested in 2020 than in 2019.
In February 2022, Kenya was one of five African co-hosts of the seventh replenishment preparatory meeting, which put “the spotlight on Africa’s leadership role in global health” and on Kenya’s achievements. The country also plays a prominent role in Global Fund governance, holding the board seat for East and Central Africa. Kenya’s former auditor-general is the current chair of the Audit and Finance Committee. Kenya has a proactive CCM on which development partners are represented by the Clinton Health Access Initiative and France. The UK stepped down from the CCM in 2020.
The performance of the Global Fund
The Global Fund is part of a global health partnership of governments, international agencies, private companies, civil society and community organisations working to improve global health outcomes. As such, the Global Fund depends on other agencies to fulfil its aims. It deliberately quotes results for the ‘partnership’ rather than for its own work. It reports that 50 million lives have been saved since 2002 due to partnership efforts to tackle the three diseases. Other partnership results cited include the following:
- Life expectancy has risen dramatically in many countries. For example, two-thirds of the increase in life expectancy in Malawi, from 46 years in 2002 to 65 years in 2019, is attributed to reduced deaths from the three diseases.
- The number of deaths each year caused by AIDS, tuberculosis and malaria has decreased by 70%, 21% and 26% respectively since 2002.
- 133 million mosquito nets were distributed by the partnership in 2021.
- In 2021, 22.3 million people accessed antiretroviral therapy for HIV, which represents an increase in people treated, despite the COVID-19 pandemic.
The Global Fund’s organisational effectiveness, impact and value for money are highly rated by external bodies. Civil society organisations consulted for this information note were very positive about the performance and impact of the Global Fund and many of them identify as part of its wider partnership. The UK government has consistently assessed the Global Fund as a high performer, scoring ‘A’ in all its annual reviews and ranking in the top three agencies in the 2016 Multilateral Development Review. The Multilateral Organisations Performance Assessment Network rated the Global Fund highly in 2016. The findings of its most recent review, published in July 2022, are also very positive, highlighting that the Global Fund continues to make substantial progress in addressing the three diseases, but needs to do better on health systems strengthening (HSS), human rights, gender and links to the Sustainable Development Goals. The Global Fund has long been challenged over whether its investments, which are short-term and have to be spent within its three-year funding cycle, do enough to help strengthen national health systems, and its approach to HSS is evolving (see Box 3). We were not able to consult recipient governments for this short information note.
Box 3: The Global Fund and health systems strengthening
The Global Fund’s structures and processes reflect its ‘three diseases’ approach, and it invests in health systems strengthening (HSS) primarily through disease-specific grants. Countries can also access designated HSS grants, with $937 million disbursed since 2002 (less than 2% of all disbursements). Overall, the Global Fund claims it is currently investing $1.5 billion a year in HSS; around one-third of its total investments. If the seventh replenishment target is met, the Global Fund anticipates investing the same proportion, equivalent to about $2 billion annually, in HSS during the upcoming funding cycle.
The Global Fund is well placed to address key gaps in capacity, for example in procurement and supply chain management, laboratory services, health information management systems and community health systems. Whether this can be achieved through disease-specific programming is unclear. The 2019 UK Global Fund Performance Agreement urges integration with “national systems and structures” and the Global Fund increasingly recognises the need to “focus on a person, not just a disease”. Its stated focus now is on building “resilient and sustainable systems for health” to deliver “people-centred, integrated systems for health” and contribute to pandemic preparedness and response.
The Global Fund relies on country systems to manage very high volumes of procurement. It seeks to strengthen these systems as an investment in the long-term sustainability of health programmes. This is a core principle of the Global Fund, supported by the UK, which has been maintained despite the pressures of COVID-19 and shortcomings in supply chain management in some countries. For example, recent Office of the Inspector General audits and investigations have highlighted significant weaknesses in commodity procurement and supply systems in Kenya and Nigeria, the two countries that we looked at more closely.
The Global Fund has developed several tools to support country procurement, including an online platform which enables countries to submit and track orders with suppliers. Countries can also use this platform to access the Global Fund’s pooled procurement mechanism (PPM), which aggregates orders for key products to secure good prices and timely delivery. Both the PPM and the online procurement platform are central to the Global Fund’s market-shaping strategy, which aims to use the Global Fund’s purchasing power to create sustainable markets for affordable, quality-assured health products.
The Global Fund and COVID-19
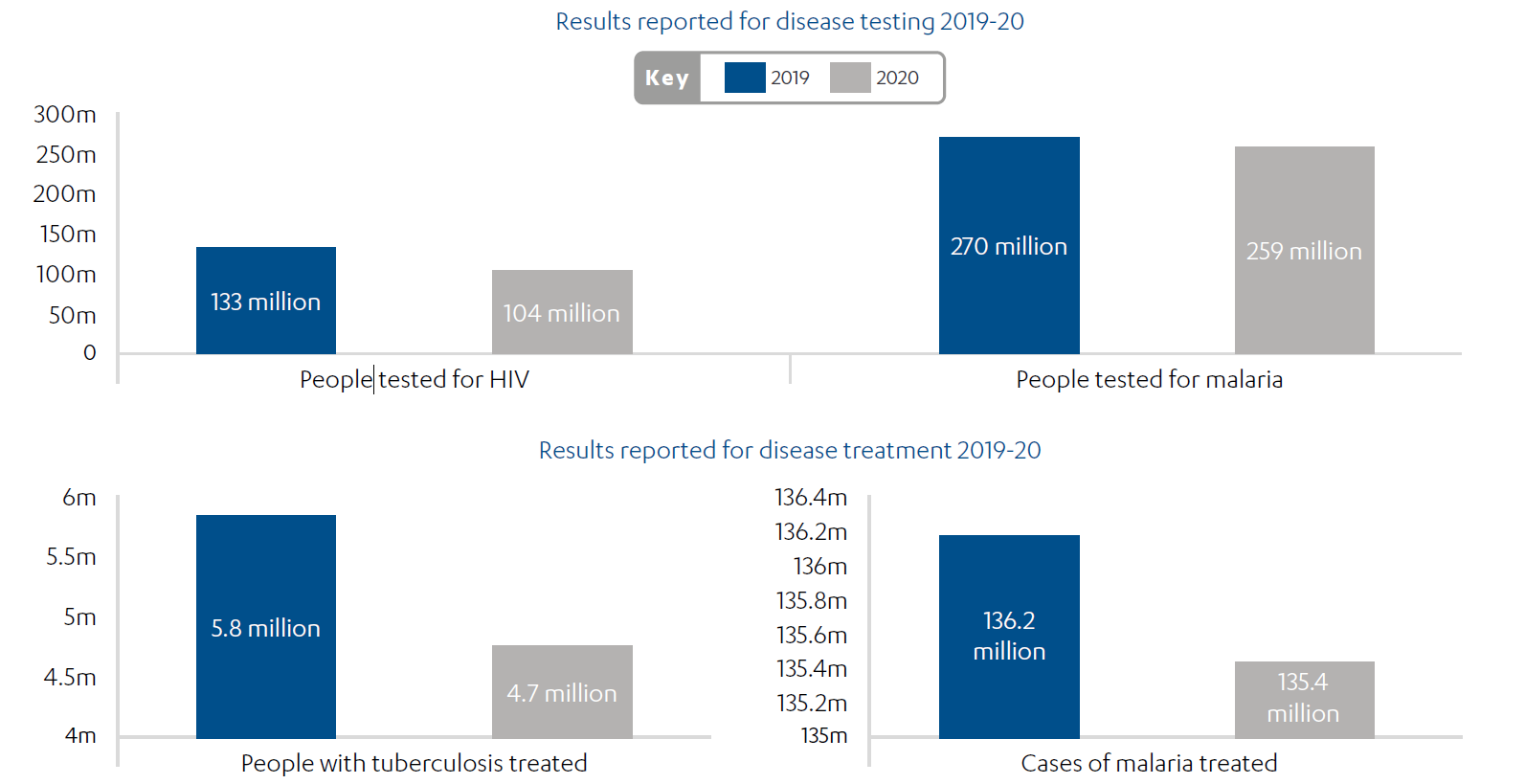
The COVID-19 pandemic has had a severe impact on the Global Fund’s efforts to curb AIDS, tuberculosis and malaria, as well as its broader impact on health systems. Most areas of testing and treatment for the three diseases have seen a decline, including significant drops in the numbers treated for tuberculosis and malaria (see Figure 2). This is the first time that key programmatic results have declined globally during the 20-year history of the Global Fund.
Figure 2: The impact of COVID-19 on global testing and treatment results
The Global Fund stepped up rapidly and at scale to fill a gap in the COVID-19 response. $500 million of existing grants were re-programmed and more than $4 billion has been raised, primarily from the US government, for a new COVID-19 Response Mechanism (C19RM). The Global Fund has used the new mechanism to support 109 countries and 22 multi-country programmes to respond to COVID-19. The Office of the Inspector General has recently completed an initial evaluation of the C19RM and assessed its design as adequate, describing it as “robust and inclusive”. The rollout was judged to be partially effective, with the report noting a rapid initial approval process, but some delays in procurement at country level.
Under this programme, the Global Fund has made significant contributions to the provision of COVID-19 testing and treatment, the supply of oxygen and personal protective equipment, and the training of health workers. It was a founding partner of the Access to COVID-19 Tools Accelerator (ACT-A), which is a global collaboration to accelerate the development and production of, and equitable access to, COVID-19 tests, treatments and vaccines. Through its market-shaping work, the Global Fund has achieved 50% reductions in the price of COVID-19 tests. However, COVID-related grant disbursement at country level has sometimes been slow. For example, Kenya used 51% of allocated funds within the original grant timelines.
The impact of the pandemic on some HIV, tuberculosis and malaria programmes has been mitigated through increased community health worker outreach, as used successfully in Nigeria (see Box 4), and the use of digital platforms. Health system investments have been expanded, for example in laboratory and diagnostic capability. The Global Fund has placed a strong emphasis on community engagement in the COVID-19 response and programme adaptations. These are evolving into a broader pandemic preparedness agenda, as featured in the Global Fund’s new strategy.
The UK’s role in the Global Fund
Improving global health is a UK priority as laid out in the Integrated review, the International development strategy and policy papers on Ending preventable deaths and Health systems strengthening. The new International development strategy mentions the Global Fund, alongside Gavi, the vaccine alliance, as two initiatives through which the UK will work towards ending preventable deaths of mothers, babies and children. However, the strategy also commits the UK to a relative reduction in funding through multilateral channels such as the Global Fund. The UK government committed to spend £500 million a year tackling malaria, through a range of interventions, between 2016 and 2021. But all bilateral programmes related to malaria are now closed, and resources for all three diseases have increasingly been channelled through the Global Fund. The UK has increased its share of total pledges to the Global Fund from 6% in 2008-10 to over 12% since 2014 (see Figure 3).
The UK pledged up to £1.4 billion to the sixth replenishment in 2019; an increase of 15% on its previous commitment, as requested by the Global Fund. As a result, it maintained its status from the fifth replenishment as the Global Fund’s second-largest donor after the US. However, since 2020, the payments for some tranches of the UK’s sixth replenishment pledge have been partially rescheduled, causing cash flow concerns for the Global Fund. In response to a Parliamentary question, the UK government stated in February 2022 that it was on track to fulfil its sixth replenishment pledge, but since July 2022 it has temporarily suspended all ‘non-essential’ aid payments.
Figure 3: UK pledges as a share of total pledges by replenishment
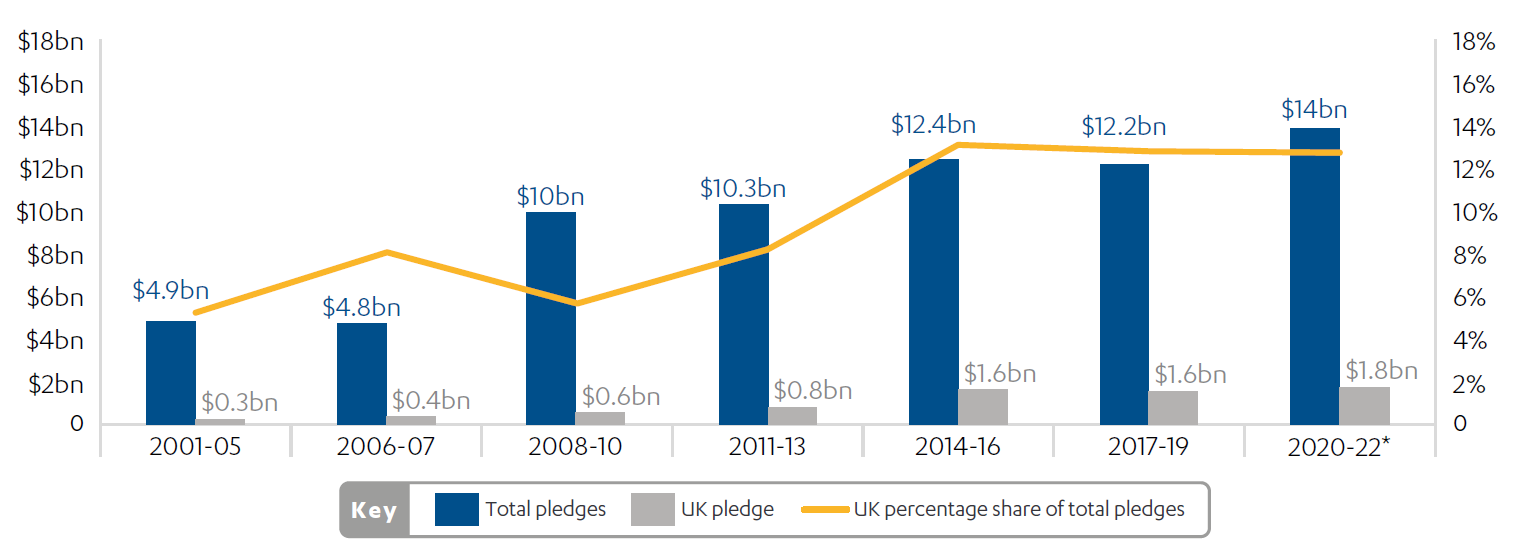
*Total pledges at sixth replenishment before C19 Response Mechanism
Source: The Global Fund data explorer – pledges and contributions, The Global Fund, accessed 7 July 2022, link; and Pledges at Global Fund sixth replenishment conference, The Global Fund, 9-10 October, 2019.
UK policy priorities for the Global Fund have been consistent in recent years and include equity and inclusion, gender, health systems strengthening, results, value for money, addressing sexual exploitation, abuse and harassment (SEAH), and pandemic preparedness. The UK is an active board member and made substantial contributions to the Global Fund’s 2023-28 strategy. The UK currently has representatives on the board committees for Ethics and Governance, and for Strategy. The UK cooperates closely with other donors, to ensure that all their views are well represented across all three board committees. Feedback on the UK’s role from other stakeholders was universally positive, stressing technical expertise and staff continuity as valuable assets in addition to its financial contributions.
The UK is not currently on the Audit and Finance Committee but was a member from 2014-22, including two years as deputy chair. The UK was a powerful voice on that committee, focused on SEAH, corporate performance and the quality of risk management. The Foreign, Commonwealth and Development Office (FCDO) judges the Global Fund’s financial controls to be strong and its external audit team to have high capacity. FCDO appreciates the responsiveness of the Global Fund to its concerns. When, for example, the UK government said that it wanted to see change on SEAH, the Global Fund started to build a team to respond.
FCDO sees its bilateral health programming and its investments in the Global Fund as being complementary. The UK has variable engagement with the Global Fund at country level. FCDO has a Health Institutions and Health Security Department, which has provided guidance and encouragement to UK embassies and high commissions on engaging in the development of funding requests for the Global Fund under the current replenishment cycle. The UK government’s membership in Country Coordinating Mechanisms (CCMs) is largely dependent on the presence of health advisers in the UK embassies and high commissions. UK input to CCMs is often through another donor, elected to represent all donors, which makes coordination vital.
key innovations in the relationship between the UK and the Global Fund, 2019-22
As part of its commitment to the Global Fund for the sixth replenishment in 2019, the UK established a performance agreement with the Global Fund covering four key areas: (i) leadership and collaboration; (ii) organisational effectiveness, including equity and sexual exploitation, abuse and harassment; (iii) impact; and (iv) sustainability. This was linked to a £100 million performance tranche, which was dependent on the Global Fund achieving certain conditions. These have been met to date. The performance agreement is monitored by the Foreign, Commonwealth and Development Office (FCDO) in annual strategic meetings and supported by more detailed indicators. The Global Fund accepts these, as they are aligned with its own corporate indicators, while noting that it would not be able to sustain the burden of such conditionality for all donors.
The UK’s sixth replenishment pledge included a malaria private sector matching fund (also included in the fifth replenishment) which helped to meet the UK government’s spending targets on malaria. The aim was to provide £200 million, based on £100 million of matching pledges from the private sector. This was rapidly achieved, including a £50 million pledge from the Bill and Melinda Gates Foundation, which the Global Fund counts as private sector funding.
The UK held back up to 5% of its overall pledge (£70 million) for a linked technical assistance programme, the Global Fund Accelerator (GFA). This practice has been used by other donors, but was new for the UK in the sixth replenishment. Elements of the GFA include:
- Two seconded advisers in the Global Fund’s headquarters in Geneva on equity and human resources for health.
- Six country-level GFA advisers who support the development and implementation of Global Fund programmes on secondment to the BACKUP Health programme. These GFA advisers also work within UK embassies and high commissions.
- Initiatives, including programming, to support market shaping, human rights, tuberculosis service access and Africa constituencies in the Global Fund.
GFA advisers in-country and in Geneva are warmly welcomed by the Global Fund. The country advisers are recognised to be undertaking high-quality work and, although only recently recruited, are already seen as important in filling gaps and raising the quality of Global Fund programmes. These posts are funded until March 2024 and may be extended as part of the UK’s contribution to the seventh replenishment.
In its role as a board member, the UK supported the Global Fund response to COVID-19 and the COVID-19 Response Mechanism (C19RM). The UK’s financial contribution to the C19RM consisted of £60 million for testing and treatment, provided in February 2022. This came late in the process and was not on the same scale as some other donors.
Box 4: Nigeria case study
Progress in Nigeria is key to meeting Global Fund objectives and Sustainable Development Goal 3.3. The country has the highest absolute number of malaria cases and deaths and the third-highest number of HIV infections globally, as well as Africa’s largest tuberculosis burden. Nigeria is accordingly the largest Global Fund grant recipient, with $3.79 billion allocated and $3.15 billion disbursed to date.
The country has seen significant progress in key areas, including dramatic increases in malaria testing and in the proportion of HIV-positive people receiving antiretroviral therapy. During the COVID-19 pandemic, service integration and outreach led to an increase in tuberculosis and HIV case detection. However, a recent Office of the Inspector General audit identified issues with reaching vulnerable populations and managing COVID-19 funds, and expressed concern about the country’s supply chain management arrangements.
FCDO now has a GFA adviser in Nigeria, who is also part of the FCDO health team and represents donors in Nigeria’s Country Coordinating Mechanism. Current priorities for this advisory role include promoting health systems strengthening, improving coordination between the Global Fund and other development partners, and informing UK engagement in the Global Fund’s board and committees.
The seventh replenishment
The Global Fund has a replenishment model, where different countries host the replenishment meeting every three years and thus have an incentive to lead the pledging process. This model has been very successful, and has led to a significant increase in resources over the course of its 20-year lifespan. The seventh replenishment takes place from 19 to 21 September 2022, hosted by the US. The Global Fund has set an ambitious $18 billion target, an increase of 30% on the previous replenishment. It projects that this will save 20 million lives and that each £1 invested will yield a return of £31. Its investment case is guided by a Modelling Guidance Group under the leadership of Imperial College London. It outlines actions required to get back on track to end the three epidemics of AIDS, tuberculosis and malaria by 2030, in line with Sustainable Development Goal 3.3. The Global Fund’s modelling estimates that even with a replenishment of at least $18 billion, and ambitious projections for domestic resource mobilisation, there will still be a gap in resources to meet needs fully, but that this level of replenishment would allow the world to get back on the trajectory required to end the epidemics by 2030.
The Global Fund sees itself as a learning organisation and the background to the seventh replenishment is the new Global Fund strategy 2023-28, which emphasises a people-centred approach. The strategy strongly reflects UK priorities including prevention of the three diseases, gender, equity, sustainability, pandemic preparedness, health systems strengthening and global health security. Key innovations of the strategy are summarised in “10 key shifts” (see Box 5 below).
Box 5: “10 key shifts” in the Global Fund strategy 2023-28
1. An intensified focus on prevention.
2. Much more emphasis on integrated, people-centred services.
3. The development and integration of community systems for health.
4. A stronger role and voice for communities living with and affected by the diseases.
5. Intensified action to address inequities, human rights and gender.
6. Greater emphasis on programmatic and financial sustainability.
7. Greater focus on accelerating innovations.
8. Much greater emphasis on data-driven decision-making.
9. Recognition of the role of the partnership in pandemic preparedness and response.
10. Clarity on the roles of partners across the strategy for mutual accountability.
The UK government did not make its pledge ahead of the seventh replenishment and is later in doing so than for the sixth replenishment. Germany and Japan have announced increased pledges. The US has pledged up to $6 billion, but will only provide a maximum of one-third of the total replenishment. This creates a ‘multiplier’ effect for other donors, both positive and negative: any pledge by another donor will unlock an additional 50% of the value of its pledge from the US, but if other donors do not collectively pledge $12 billion, the US contribution will fall to ensure that its overall contribution remains at one-third. The Global Fund also needs to manage its cash flow and is affected by the timing of any contributions.
UK civil society organisations are campaigning for a UK contribution of £1.8 billion, in line with the aggregate funding request from the Global Fund. The UK government makes its pledge against a backdrop of reduced aid resources resulting from its decision in November 2020 to reduce official development assistance from 0.7% to 0.5% of gross national income. The shortage of resources for aid has been exacerbated by unanticipated calls on the humanitarian budget relating to Ukraine, among other issues, which led in the second half of July 2022 to a temporary suspension of ‘non-essential’ aid payments. The UK’s new pledge to the Global Fund is also being made in the context of the International development strategy’s objective to reduce the UK’s proportion of multilateral spending. The UK government therefore has had to make difficult choices between institutions in its funding of the global health system and to balance its bilateral and multilateral funding for health to achieve its overall global health objectives.
The UK needs to bear in mind:
- the multiplier effects of its pledge on the US contribution
- the incentive effects of UK actions for other donors
- the impact of its pledge on its role and influence within the Global Fund
- the consequences for health outcomes if the replenishment target is missed.
Looking ahead, the Global Fund’s ability to deliver its 2023-28 strategy will have a bearing on the UK’s objectives for global health. For example:
- Global health security: due to COVID-19, one million fewer people were treated for tuberculosis during 2020, each of whom could infect up to 15 further people within a year, while multi-drug resistant tuberculosis remains a pandemic threat. Tuberculosis programming is heavily reliant on the Global Fund.
- Ending preventable deaths: adolescent girls and young women remain particularly vulnerable to HIV infection, while malaria remains a leading cause of illness and death among children under five.
- Health systems strengthening: the Global Fund’s new emphasis on supporting integrated health services (see shifts 2 and 3 in Box 5 above) could help health workers and facilities respond to all diseases and health issues, offering potential for increased efficiency and impact.
- Science and technology: the Global Fund plays a key role in enabling access to new health technologies and stimulating further investment in innovation.
Suggested lines of enquiry for future scrutiny
We conclude by suggesting lines of enquiry that the International Development Committee or other scrutiny bodies may wish to pursue:
- Multilateral commitments: Can FCDO square a large reduction in the proportion of multilateral spending with its reliance on the Global Fund to meet its global health objectives, and particularly Sustainable Development Goal 3.3?
- Women and girls are disproportionately affected by HIV and malaria. What is the Global Fund’s role within the government’s objectives for women and girls?
- Global health ecosystem: How does FCDO’s support for the Global Fund interact with support to other global health initiatives? What complementary investments should the UK make to maximise Global Fund performance and impact?
- Value for money and the private sector: How can FCDO continue to use the Global Fund to maximise the value for money of its health investments, deliver cost savings through market shaping and leverage private sector investment in tackling malaria and other health challenges?
- Global health security and pandemics: What role does FCDO believe that the Global Fund should play in preventing and responding to future pandemics and strengthening overall global health security?