The UK aid response to global health threats
ICAI score
A relevant and coherent strategy for responding to global health threats. There is good potential for programmes to be effective, particularly if better integrated with health systems strengthening, but the approach to building learning and sharing knowledge is weak.
The UK government responded rapidly to weaknesses in the international response system exposed by the Ebola crisis, developing a coherent and evidence-based framework for addressing global health threats and establishing a portfolio of relevant and often pioneering programmes and influencing activities.
The portfolio shows strong potential to be effective, particularly on influencing WHO reform, building surveillance systems in high-risk countries, developing new vaccines and supporting a timely response to contain new outbreaks. Cross-government mechanisms for sharing global health threats data and deciding how to respond also show signs of promise.
Building on this strong foundation, there is an opportunity for DFID, the Department of Health and other relevant bodies to do even better. There is a need to update the global health threats strategy and communicate it more widely. There should be better coordination across centrally managed programmes and with DFID country offices and there should be a greater emphasis on strengthening country health systems across all programming.
The government’s approach to generating and sharing evidence on what works is weak. Improvements are needed to secure what has been achieved to date and to support the effectiveness and value for money of future efforts to tackle global health threats.
| Individual question scores | |
|---|---|
| Question 1 Relevance: Does the UK have a coherent strategy for using aid to address global health threats? |  |
| Question 2 Effectiveness: Is the emerging aid portfolio a potentially effective response to global health threats? |  |
| Question 3 Learning: Is learning informing the continuing development of the UK aid response to global health threats? |  |
Executive Summary
The Ebola crisis from 2014 to 2016, which killed more than 11,000 people, brought a new level of urgency to the issue of global health threats – infectious disease outbreaks and drug resistance with the potential to spread across borders. The Ebola outbreak led to a protracted humanitarian emergency and severe developmental setbacks in Guinea, Liberia and Sierra Leone, and spread panic and disruption to trade and travel far beyond West Africa. It exposed weaknesses in epidemic preparedness and response, and highlighted failings within the World Health Organization (WHO) and across the international health emergency response system. The crisis also demonstrated the fundamental challenge of responding effectively to global health threats in countries with weak national health systems.
While health has been a major focus of UK aid for many years, the response to and lessons from the Ebola crisis stimulated a rapid scaling up of activity and spending to address global health threats. An additional £477 million was allocated to the Department of Health in the spending period 2016-21 to support this activity, while the Department for International Development (DFID) has also scaled up its efforts. The government’s aim is to reduce the risk of future outbreaks, to support countries and the international community to better prepare for them, and to improve the international response when outbreaks occur.
In this learning review, we gauge how successful this rapid scaling up of aid activity has been. We look at how the UK government has developed a strategy and a portfolio of programmes on global health threats, building in particular on the lessons learnt from the Ebola outbreak. We assess how effectively it has implemented this strategy, and how it is using learning to inform future activity. Throughout the review, we consider how evidence, knowledge generation and learning have been translated into strategy, programming and global influencing. For the purpose of this review, we understand global health threats to include infectious disease epidemics that risk spreading across borders and emerging diseases with epidemic potential, as well as the threat posed by drug-resistant microbes. This is in line with the priorities of the 2015 UK aid strategy.
The scope of our review is broad, reflecting the range of activities developed by the government as part of the UK aid response to global health threats. Given the cross-government nature of this response, the review looks specifically at the effectiveness of collaboration between the different departments and agencies involved.
Relevance: Does the UK have a coherent strategy for using aid to address global health threats?
As the Ebola crisis unfolded, the UK government moved quickly to diagnose the challenges and failings in global health threats preparedness. The Department of Health and DFID drew on this evidence base and responded with a shared strategic framework, Stronger, Smarter, Swifter, underpinning a portfolio of programmes and interventions. The framework was focused on stronger health systems, smarter development of new vaccines, diagnostic tools and detection of drug resistance, and swifter response to outbreaks and epidemics. We found that the strategy provided a relevant and well-balanced framework for action, and each of the major global health threats programmes we reviewed was supported by a strong strategic rationale.
This strategic framework has provided a strong foundation for the government’s programming on global health threats since 2015. We nevertheless found room for improvement. The framework could provide greater clarity on the roles of different government departments, and on the cross-cutting importance of health systems strengthening. The strategy could also articulate a broader range of research priorities, beyond vaccine and product development. At country level, the degree to which DFID country offices have prioritised global health threats objectives has been mixed. Meanwhile, centrally managed global health security interventions (including those focused on antimicrobial resistance) would benefit from a more explicit cross-programme focus on health systems strengthening, since robust national health systems are critical to the task of detecting, responding to and containing global health threats.
Stronger, Smarter, Swifter was intended primarily for internal use and has not been published. With a number of donors and multilateral agencies entering or scaling up their activity in this area, we see an increasing need for the UK government to communicate and promote its strategy more clearly in order to help and encourage other donors and investors to align their activities and spending with the UK’s efforts.
Overall, we have awarded the UK government’s global health threats strategy a green-amber score for relevance. This recognises the considerable achievement in the wake of the Ebola crisis of developing a coherent framework for addressing global health threats, backed by strong evidence of need, as well as a relevant portfolio of programmes and influencing activities. However, there is a need to build greater linkages between the government’s global health threats work and strengthening national health systems. And also to clarify and improve cross-government ways of working, and to disseminate the strategy externally.
Effectiveness: Is the emerging aid portfolio a potentially effective response to global health threats?
The UK has a portfolio of potentially impactful programmes. Programmes managed centrally by both DFID and the Department of Health have made positive progress to date. DFID’s country health programmes are generally contributing to strengthening the disease surveillance mechanisms of country health systems and improving the resilience of health systems to future disease outbreaks.
Overall, the UK has shown international leadership on global health threats. It has been influential in encouraging the WHO to reform and securing global policy commitments on antimicrobial resistance. The Department of Health and DFID have collaborated effectively to promote improved international data gathering and assessment mechanisms during disease outbreaks.
There remain areas for improvement. The UK’s influencing strategy has had little success in encouraging other donors to invest in the WHO Health Emergencies Programme. At country level, global health security programmes could do more to support comprehensive health systems strengthening, working closely with partner governments to ensure that interventions to tackle specific diseases and health issues also contribute to the quality and robustness of national health systems. Other ODA-funded global health research has yet to be fully aligned with the global health threats agenda, missing opportunities to encourage joined-up medical and social science research responses.
There is a general need for improvements in cross-government collaboration and communication. At the strategic level, we found that oversight mechanisms could provide stronger leadership and coordination to all government departments with global health security programmes and expertise. At the programme level,
country offices and centrally managed programmes need better coordination, and country offices would benefit from increased capacity to coordinate UK aid-funded interventions and influencing activities.
Overall, we have awarded a green-amber score for effectiveness. This recognises that the global health security portfolio shows strong potential to be effective.
Learning: Is learning informing the continuing development of the UK aid response to global health threats?
Having been quick to capture lessons from the Ebola crisis and build these into its Stronger, Smarter, Swifter strategic framework, the UK government has not followed through with sufficiently robust evaluation and knowledge dissemination practices.
A variety of UK government and external stakeholders we talked to commented on the need to improve learning and knowledge sharing. With some exceptions, mechanisms to evaluate programmes and to share learning are inconsistent or underdeveloped. We found evidence of some good monitoring and learning practices within individual programmes, but not enough dissemination of lessons beyond the programmes generating them, or between government departments. In the country programmes we reviewed, we saw little evidence that lessons were shared more widely. We also found that there is currently no overarching evaluation and learning strategy to support the Stronger, Smarter, Swifter framework.
We have given the government an amber-red score on learning, noting that improvements are needed to build on the achievements to date and to support the effectiveness and value for money of future efforts to tackle global health threats.
Conclusions and recommendations
We have given the UK government an overall score of green-amber for its aid effort to tackle global health threats since the Ebola outbreak. The government has made good progress in developing a coherent framework for addressing the risks from infectious disease outbreaks and drug resistance, as well as rapidly establishing a relevant portfolio of programmes and influencing activities. Nevertheless, our review highlighted some gaps and a number of opportunities for improvements.
The following recommendations are intended to help the government, and the Department of Health and DFID in particular, to further improve its strategy and interventions.
Recommendation 1
The UK government should build on the success of the Stronger, Smarter, Swifter framework by developing a refreshed global health security strategy with a clearer focus on strengthening country health systems, a broader set of research priorities and clearly defined mechanisms for collaboration both across departments and with external actors. The strategy should be published and communicated widely.
Recommendation 2
The Department of Health and DFID should strengthen and formalise cross-government partnership and coordination mechanisms for global health threats, broadening their membership where relevant. This should include regular cross-government simulations to rehearse how the UK government might coordinate and respond internationally to a future global health threats crisis similar to Ebola, and engage with other actors such as the WHO.
Recommendation 3
The government should ensure that DFID has sufficient capacity in place to coordinate UK global health security programmes and influencing activities in priority countries, including around the objective of strengthening national health systems.
Recommendation 4
DFID and the Department of Health should work together to prioritise learning on global health threats across government, overseeing the development of a broad evaluation and learning framework, regular reviews of what works (and represents good value for money) across the portfolio, and a shared approach to the training and development of health advisors.
Introduction
Purpose
Global health threats are of increasing concern to the international community and to the UK government. Infectious disease outbreaks and drug resistance, with the potential to spread across borders, feature prominently in the UK aid strategy and the National Security Strategy and Strategic Defence and Security Review, both published in 2015.
Global health threats present a direct challenge to the overarching aims of the government’s aid strategy: to support international development while at the same time protecting the UK’s national interest. Certain diseases with epidemic potential, such as Ebola, influenza, severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), are a threat not just to affected countries but also to the international community due to their high fatality rate, the risk that they will spread internationally and their potential to cause panic, disruption and disorder.
The 2014-16 Ebola crisis in West Africa saw borders closed and severe disruption to international trade and travel. The World Health Organization (WHO) declared the outbreak a Public Health Emergency of International Concern. By the time it lifted this designation in March 2016, Ebola had killed more than 11,000 people – one in every three people infected – in the three countries worst affected by the outbreak (Guinea, Liberia and Sierra Leone).
The emergency led to a protracted humanitarian crisis. It also had a severe developmental impact in these countries. It placed already weak health systems under extreme pressure, leading to an initial failure to contain the outbreak. GDP growth collapsed, while consumption, employment and school attendance rates fell. The World Bank estimates that the Ebola outbreak cost the economies of Guinea, Liberia and Sierra Leone, already among the world’s poorest, at least US$2.8 billion in lost growth.
Box 1: How this report relates to the Sustainable Development Goals
The Sustainable Development Goals (SDGs), otherwise known as the Global Goals, are a universal call to
action to end poverty, protect the planet and ensure that all people enjoy peace and prosperity
Related to this review
![]()
Ensure healthy lives and promote well-being for all at all ages
SDG3 sets out to end the epidemics of AIDS, tuberculosis, malaria and other communicable diseases by 2030. Crucial to achieving this goal is to strengthen national health systems and provide quality treatment for everyone, including the poorest and most vulnerable in society. Better quality health systems also strengthen countries’ capacity for early detection and warning, and improve their ability to contain and manage outbreaks. Research and development of new vaccines, and the provision of these and good quality medicines at affordable prices, is also central to SDG3.
Combating global health threats is recognised as central to achieving the SDGs. As our description of the Ebola crisis in this review makes clear, health emergencies do not only have health impacts. They affect a range of SDGs, from health to education and jobs, economic growth and poverty alleviation.
While health has been a major focus of UK aid for many years, the response to and lessons learnt from the Ebola crisis prompted a rapid scaling up of activity to address a range of global health threats. An additional £477 million was allocated to the Department of Health to support this activity in the spending review period 2016-21. The Department for International Development (DFID) also scaled up its activity on global health threats,
developing new strategies and programmes, refocusing some of its existing spending and ramping up its global influencing and advocacy work.
The government’s objectives, summarised in the UK aid strategy, are to:
- reduce the risk of future outbreaks
- support countries and the international community to better prepare for outbreaks
- improve the international response when outbreaks occur.
Since this is a relatively new policy area, with a rapid scaling up of investments, we decided to conduct a learning review (see Box 2) of how the UK government developed its framework and portfolio of programmes on global health threats, how it has implemented this strategy and how it is using learning to inform future activity. Throughout the review, we consider how evidence, knowledge generation and learning have been translated into strategy, programming and global influencing activities.
Box 2: What is an ICAI learning review?
ICAI learning reviews examine new or recent challenges for the UK aid programme. They focus on knowledge generation and the translation of learning into credible programming. Learning reviews do not attempt to assess impact. They offer a critical assessment of progress to date and whether programmes have the potential to produce transformative results. Our learning reviews recognise that the generation and use of evidence are central to delivering development impact.
Other types of ICAI reviews include impact reviews, which examine results claims made for UK aid to assess their credibility and their significance for the intended beneficiaries, performance reviews, which examine effectiveness and value for money, and rapid reviews, which represent short, real-time reviews of emerging issues or areas of UK aid spending of particular interest to the UK Parliament and the public.
Scope
The UK’s response to the growing risk of global health threats has been wide-ranging. Two departments, DFID and the Department of Health, have taken the lead, but other departments and agencies, including the Cabinet Office and Public Health England, have also had important roles. Our scope covers the totality of the UK aid response to global health threats, regardless of the spending department.
In line with the UK aid strategy, we understand global health threats to include infectious disease epidemics that risk spreading across borders and emerging diseases with epidemic potential, as well as the threat posed by drug-resistant microbes (often referred to as the challenge of antimicrobial resistance). Some definitions of global health threats include the accidental or deliberate release of diseases, chemical and nuclear hazards, and non-communicable diseases. However, these are outside the scope of our review.
Within this focus on epidemic threats and antimicrobial resistance, our review explores the UK’s support for emergency preparedness and response. This includes the government’s contribution to influencing and strengthening international systems for health surveillance and crisis response, such as the International Health Regulations (see Box 4). In addition, the review explores how new areas of emphasis in addressing global health threats are balanced with the longer-term process of strengthening the national health systems of developing countries.
The questions guiding our review are outlined in Table 1.
Table 1: Our review questions
| Review criteria and questions | Sub-questions |
|---|---|
| 1. Relevance: Does the UK have a coherent strategy for using aid to address global health threats? | • Are investments prioritised according to the emerging evidence and assessments of the health risks to partner countries and the UK? • Do UK aid investments follow a coherent strategy or approach? |
| 2. Effectiveness: Is the emerging aid portfolio a potentially effective response to global health threats? | • Is UK aid providing effective support for the strengthening of international systems of prevention and management of global health threats? • Is UK aid providing effective support for the building of national health systems preparedness for global health threats? • Is there effective joint working and coordination across the UK government? |
| 3. Learning: Is learning effectively informing the aid portfolio’s response to global health threats? | • Are there effective learning and dissemination mechanisms in place? |
Methodology
The diagram below outlines our approach to the review. The four main elements to our methodology were: a literature review, a strategy review, case studies and programme reviews.
Figure 1: Our methodology approach
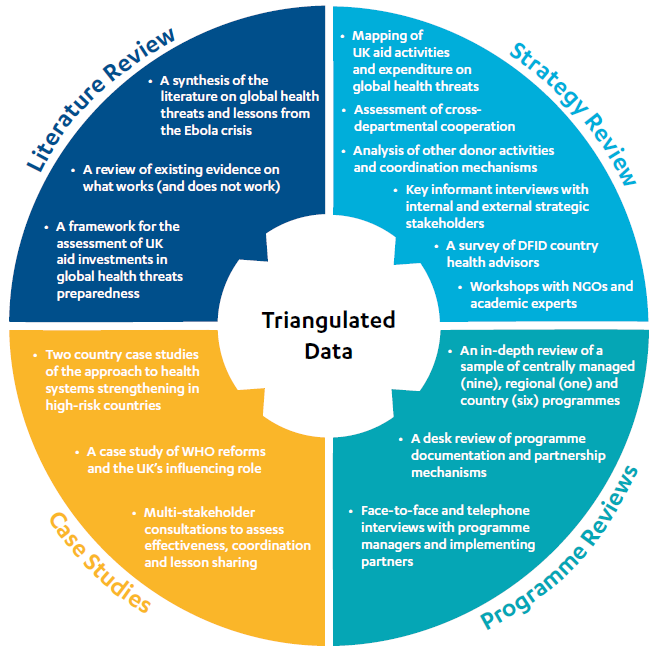
Our literature review explored definitions of global health threats, views on the nature of these threats, perspectives on the international health system and its weaknesses, and the key lessons learnt from the Ebola crisis. It also considered evidence on effective practice in addressing global health threats. The literature review provided a reference point to assess the relevance, coherence and emerging effectiveness of UK aid investments.
In our strategy review, we mapped the response of the key departments involved with the UK government’s approach to addressing global health threats. This informed our assessment of: the relevance of the UK strategy; its added value; the visibility and coherence of the approach; its emerging effectiveness (including influencing and leveraging other actors’ contributions); the effectiveness of cross-government and external coordination; and the degree of ongoing learning and dissemination activity underway.
The strategy review drew on:
- desk studies of strategies, programmes and expenditure
- key informant interviews with UK government representatives and wider stakeholders, including from other bilateral donors, the WHO, philanthropic organisations (such as the Wellcome Trust and the Bill & Melinda Gates Foundation) and pharmaceutical companies
- an email survey of DFID country health advisors
- two workshops, one with non-governmental organisations and one with academic experts.
We conducted programme reviews of a sample of nine interventions drawn from centrally managed programmes developed by DFID and the Department of Health, and six country-level programmes managed by DFID. The sample was drawn from the list in Annex 2 of all the programmes that we identified as relevant to global health threats.
To expand on insights generated by our programme reviews, we undertook two country case studies. We visited Burma and Sierra Leone to assess: the relevance of UK aid investments there; progress in their implementation; and lessons learnt from them. The country visits were complemented by a visit to the WHO headquarters in Geneva to examine efforts to support WHO reform and gather further perspectives on the UK aid response to global health threats. As part of these case studies, we spoke to a range of stakeholders including from the UK and partner governments, other donors and multilateral institutions.
Both our methodology and this report were independently peer reviewed.
Box 3: Limitations of our methodology
Our case studies and programme reviews were purposively selected to reflect a range of relevant contexts and programme types. The sample may not be fully representative, and caution should be applied to generalising all our findings to the UK government’s response to global health threats as a whole.
Given the review timescales, our literature review did not assess all relevant literature. Rather, we prioritised key sources based on an initial analysis of the likely significance and relevance of each source. As a result, some potentially relevant sources may not have been included.
As the scaled-up government response to global health threats in the wake of Ebola is relatively new, there was limited availability of independent evaluations and academic reviews of the government’s approach. Our review therefore relied on combining evidence from stakeholder perspectives and other sources with our own judgements of the available evidence, rather than drawing on fully evaluated and peer reviewed assessments of progress.
Background
Global health threats and the lessons from Ebola
The Ebola crisis brought the issue of global health threats into sharp relief. It exposed weaknesses in epidemic preparedness and response, and highlighted specific failings within the WHO and across the international health emergency response system. The crisis also demonstrated the fundamental challenge of responding effectively to global health threats in countries with weak national health systems, which are unable to comply with the detection and reporting standards of the International Health Regulations (see Box 4).
Box 4: The role of WHO and the International Health Regulations in epidemic preparedness and response
WHO
WHO, the UN’s health agency, is a key international actor in the field of global health threats. It provides technical guidance and support to governments and national health systems, shapes research agendas, sets international norms and standards, and monitors national and international action on global health priorities. It houses the Global Outbreak Alert and Response Network, established in 2000 to facilitate rapid outbreak responses by coordinating and deploying experts.
WHO is funded through a combination of assessed contributions (or membership fees) and voluntary donations. Its regional offices in Africa, the Americas, South East Asia, Europe, the Eastern Mediterranean and the Western Pacific support member states in generating health data, delivering health care, and managing health services at national and sub-national levels.
The World Health Assembly brings together the 194 WHO member states and is the WHO’s supreme decision-making body. The WHO executive board, with its 34 elected technically qualified individuals, advises on and facilitates World Health Assembly decisions.
The International Health Regulations
The International Health Regulations, developed under WHO auspices in 1969 and updated in 2005, are a legally binding agreement between 196 countries, committing them to build their own national capacities to detect, assess and report public health emergencies.
The regulations focus on the effectiveness of country disease surveillance and data reporting systems. WHO uses a voluntary joint external evaluation tool to monitor and evaluate how well countries conform to the regulations.
The experience of Sierra Leone, the country with the highest infection rates in the 2014-16 Ebola epidemic, illustrates how the outbreak developed, the resulting challenges and their impacts (Box 5).
Box 5: The Ebola crisis in Sierra Leone
WHO confirmed the first Ebola cases in Sierra Leone in May 2014, with 15 cases confirmed by June.8 The government closed its borders with Guinea and Liberia, along with a number of schools. Soon after, Médecins Sans Frontières (MSF) reported that the outbreak was out of control. On 31 July, the Sierra Leone government declared a state of emergency. On 8 August, WHO declared the Ebola outbreak to be a Public Health Emergency of International Concern.
The outbreak peaked in October 2014, with cases reported in every district of Sierra Leone. By the time the WHO lifted the Public Health Emergency in March 2016, Ebola had killed 3,956 people in the country, just under one in three of those infected. Many survivors require ongoing, often intensive support to deal with the physical, social and psychological effects of their infection.
The outbreak quickly overwhelmed the health systems’ ability to respond. The UN’s Special Envoy on Ebola, David Nabarro, described how:
Ebola Treatment Units (ETUs) were full and indeed you were often in an ETU and seeing people arrive and being turned away because there was no place to be treated. Mortuaries were full, overflowing with bodies…There was a sense, not just of despair, but of abandonment.
Bringing the outbreak under control required concerted action by governments, charities, donors and multilateral organisations. The UK, the United States and France played pivotal roles in the response. Strong support for WHO from agencies and donors such as UNICEF and DFID was acknowledged to have made “an immediate large-scale difference”.
Interventions that helped bring the crisis under control were multifaceted and included:
- funding to build new treatment centres and deliver equipment
- improving the speed of quarantine procedures and access to treatment centres
- working with affected communities to develop new isolation processes
- improving the equipment and safety training available to health workers and burial teams
- accelerating the availability of medicines
- logistical support from, among others, the UK military
- improving community engagement and education
- ensuring the availability of food and supplies to affected communities and households.
While Ebola focused the world’s attention on the threat of epidemics, concern about global health threats had been high among policy makers for some time. Infectious diseases are major killers: in 2015, lower respiratory infections accounted for 3.2 million deaths worldwide. Tuberculosis (TB) caused an estimated 1.4 million deaths, while HIV-AIDS killed 1.1 million and malaria killed 429,000.
Drug resistance heightens the threat of such diseases by reducing the effectiveness of available treatments. Globally, 480,000 people develop multi-drug-resistant TB each year, and drug resistance complicates the fight against AIDS and malaria. The government-commissioned Review on Antimicrobial Resistance (known as the O’Neill review) gives a conservative estimate of 700,000 deaths per year caused by drug resistance globally, a figure that could rise to 10 million a year by 2050.
The economic costs of global health threats are also clear. Six major zoonotic disease outbreaks (infectious diseases beginning in animals and spreading to humans) in the period between 1997 and 2009 were estimated to have cost the world more than US$80 billion. Modelling commissioned as part of the O’Neill review suggests that, between now and 2050, the world can expect to lose between US$60 and US$100 trillion in economic output if drug resistance is not addressed.
Global health threats: the UK aid response
The 2015 UK aid strategy, published during the Ebola crisis, recognised that global health threats are a key challenge to British interests and international development, and included “strengthening resilience and response to crises” as a key objective. The rapidly scaled-up cross-government response global health threats was to a large extent based on the lessons from the Ebola outbreak (see Box 6).
Box 6: Lessons and insights from the Ebola crisis
The many reports investigating what went wrong during the Ebola crisis generally agree on the main weaknesses in the national and international outbreak response:
- Weaknesses in the international public health systems: International agencies and DFID relied on WHO surveillance systems, but the outbreak was declared after it was already out of control. Overall, international organisations had limited capacity to respond quickly.
- Weaknesses in national health systems: Weak national health systems in Sierra Leone, Liberia and Guinea lacked the capacity to recognise and contain outbreaks. These countries initially played down reports of Ebola due to fear of economic consequences.
- Poor communication: Community engagement was weak and public information campaigns sometimes counterproductive, discouraging people from seeking medical help.
- Lack of research readiness: Since Ebola had not been identified as a priority disease, the global health research community was not research-ready from the outset. It nevertheless geared up clinical trials for vaccines, treatments and diagnostics swiftly.
- Slow mobilisation of funding: Large-scale funding for the Ebola crisis was mobilised once developed countries felt under direct threat. Much smaller earlier investments in prevention could have averted the crisis.
- Lack of expert readiness: The speed and scale of the international response necessitated the mobilisation of staff who did not necessarily have the required expertise.
- Poor early coordination: Because it was labelled a health crisis, not a humanitarian emergency, coordination structures were ad hoc, and non-health aspects of the crisis response were poorly coordinated, particularly in the early stages.
The Department of Health and DFID are the two main departments charged with delivering the UK’s aid agenda on global health threats. Public Health England, an executive agency of the Department of Health, is also central to the UK aid effort because of its internationally recognised public health expertise. The Cabinet Office plays a coordinating role during new outbreaks and health crises.
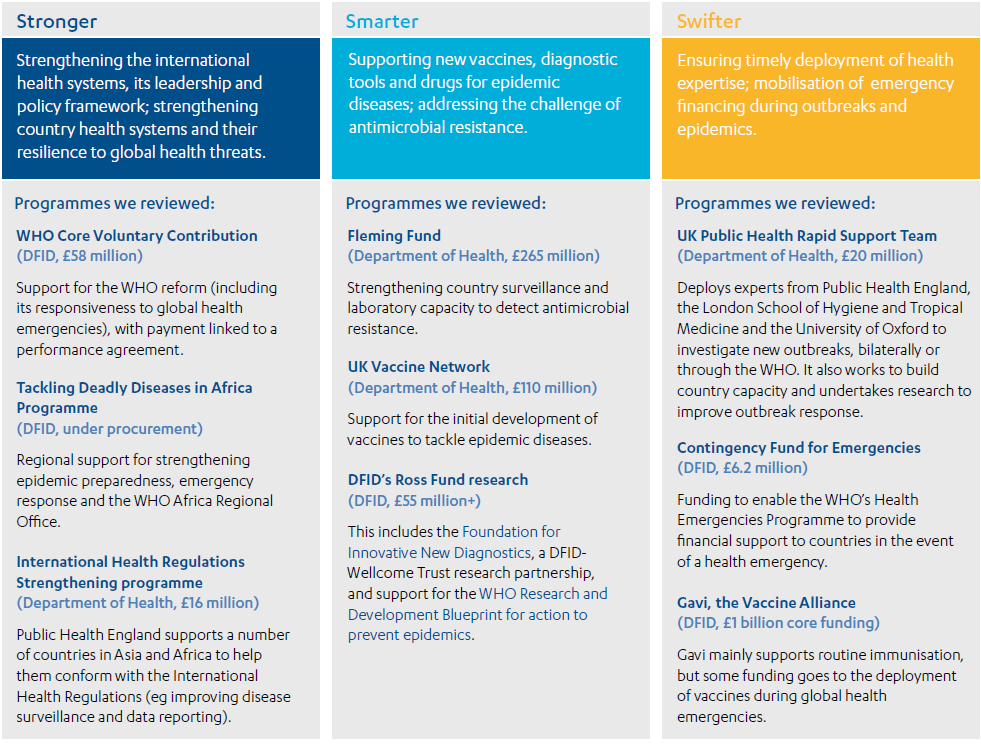
A new strategic framework for addressing global health threats, Stronger, Smarter, Swifter, was developed jointly by the Department of Health and DFID in 2015. Several centrally managed programmes align with this strategic framework (see Annex 2), with a total investment value so far of £631 million in the current spending review period (2016-21). Of this, £103.9 million is being invested in Stronger programmes, £500.9 million in Smarter, and £26.2 million in Swifter. Another £1 billion of core funding has been allocated to Gavi, the Vaccine Alliance (2016-20), although not all of this is spent on global health threats activities. Further relevant programmes are expected to come onstream from DFID in 2018.
Figure 2 lists the centrally managed programmes we selected for in-depth investigation, and outlines how they fit into the Stronger, Smarter, Swifter framework.
Figure 2: The centrally managed programmes we reviewed and how they fit into the Stronger, Smarter, Swifter strategic framework
Of the £631 million, £477 million can be clearly identified as additional spending on global health threats, corresponding with the Department for Health’s 2016 ODA allocation for its global health security programme. DFID was already making relevant investments prior to the Ebola crisis (for example in drug-resistant malaria in South East Asia), but has scaled up its work on epidemic threats and WHO reform. This includes over £50 million allocated to regional programmes in Africa and £6.2 million to strengthen the WHO’s response to health emergencies, with further investments in the pipeline.
Much of DFID’s country-level health work also furthers the global health threats agenda, even if not always as a primary goal. For instance, health systems strengthening programmes are crucial for the detection, treatment and containment of epidemic outbreaks. The lack of disaggregated spending data means we are unable to say how much country-level health spending goes specifically to activities tackling global health threats. Nevertheless, this expenditure, together with the scaled up centrally managed programmes addressing global health threats, accounts for a significant proportion of the total UK ODA budget for expenditure in the health sector of £9 billion over the period 2016-21.
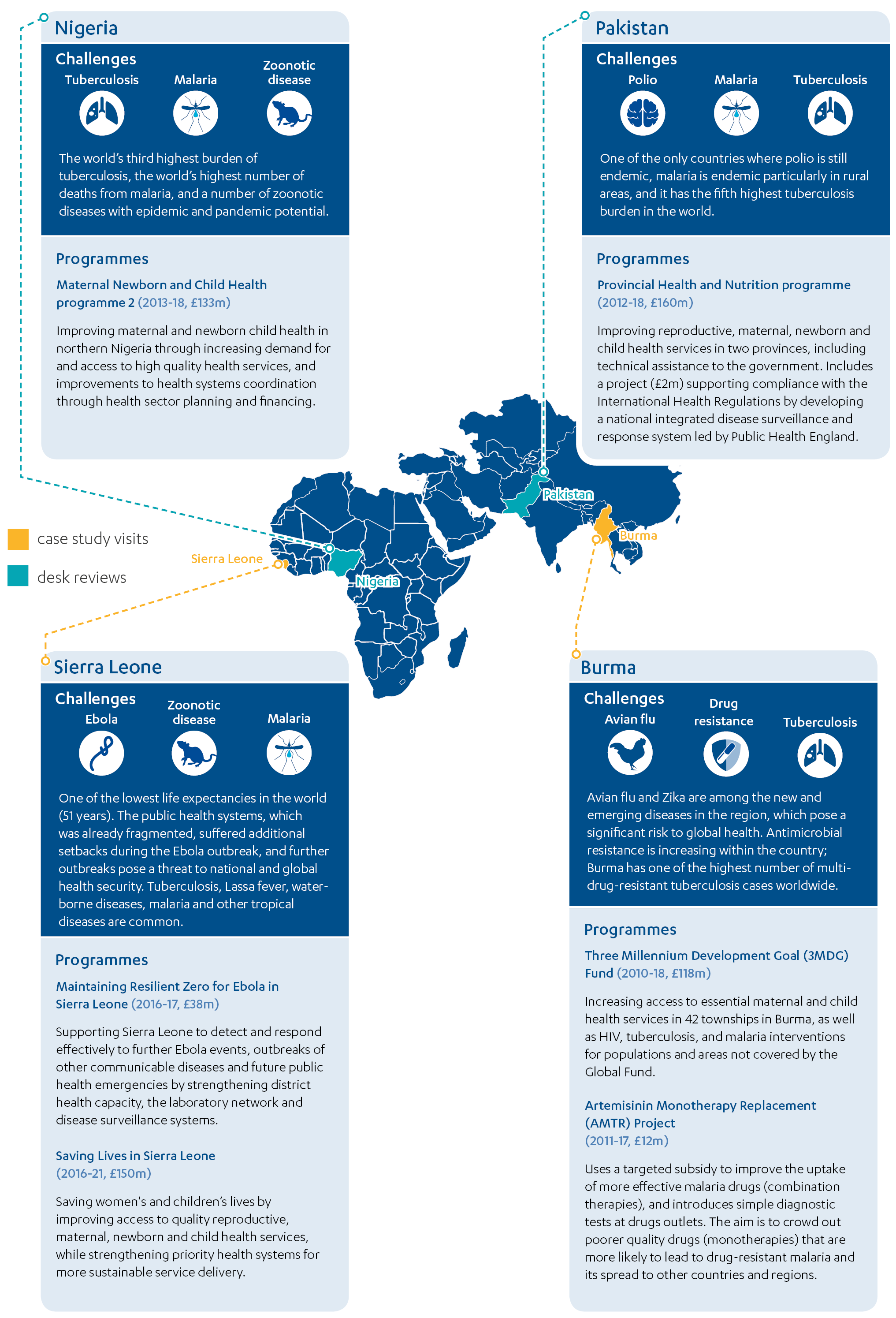
DFID has identified nine countries with global health threats activities within its country programmes. We selected six programmes from four of these priority countries for more in-depth review (see Figure 3). We made case study visits to Burma and Sierra Leone to review four of the programmes and conducted desk studies of the two programmes in Nigeria and Pakistan.
Figure 3: DFID country programmes assessed by the review
The UK’s strategy includes a range of international influencing objectives, recognising that its success relies on encouraging other countries, donors and non-governmental organisations to commit to and invest in global health threats preparedness (see Box 7).
Box 7: International influencing objectives within Stronger, Smarter, Swifter
Stronger
- international policy leadership on health systems strengthening
- WHO reform and improved global coordination
- promote the International Health Regulations
- secure commitments to health data sharing.
Smarter
- promote the antimicrobial resistance global action plan
- co-create and secure a UN General Assembly resolution on antimicrobial resistance.
Swifter
- strengthen WHO’s Global Outbreak Alert and Response Network (Box 4)
- secure financial contributions to the WHO Contingency Fund for Emergencies
- influence the design of the World Bank’s Pandemic Emergency Financing Facility.
Governance and coordination mechanisms
The governance of the UK’s Stronger, Smarter, Swifter agenda is spread across a number of government departments and bodies. At the top sits a global health oversight group, convened in 2016, with representatives from DFID and the Department of Health. It oversees global health policy and programming of mutual interest between government departments, including the cross-government response to global health threats. However, formal accountability for global health security programming lies with individual departments.
The global health security programme board is the formal governance mechanism overseeing the work carried out under each project within the global health security programme in the Department of Health. Some of the programmes have their own project boards (including some with DFID representation), which feed into the programme board.
A joint DFID-Department of Health global health research working group began meeting in 2017 to coordinate ODA-funded research on global health. A high-level steering group oversees implementation of the UK’s antimicrobial resistance strategy. A new Strategic Coherence of Official Development Assistance-funded Research Board (SCOR) was announced in September 2017, tasked with coordinating development priorities across all ODA-funded research.
DFID and the Department of Health (with Public Health England) have responsibility for the majority of programming and influencing work, but since global health threats is a cross-government priority, other departments and agencies also play a role:
- The Cabinet Office coordinated the government response to the Ebola crisis and the subsequent lesson-learning process that informed Stronger, Smarter, Swifter. The Cabinet Office’s Civil Contingencies Secretariat is responsible for emergency planning, which supports the government’s COBRA emergency response committee. In 2017, the secretariat established the International Health Risks Network, with cross-departmental representation, to help determine the UK’s response to new international disease outbreaks.
- The Government Office for Science produces the International Forward Look bulletin, which collates cross-government intelligence on international threats and disasters, including health threats, and shares these with the International Health Risks Network.
- The Department for Business, Energy and Industrial Strategy oversees the Newton Fund and the Global Challenges Research Fund (GCRF), through which much ODA funding for research on global health threats is channelled.
- The Foreign and Commonwealth Office contributes to the government’s international influencing work, including with the G7, G20 and WHO.
- The Department for Environment, Food and Rural Affairs (particularly its Veterinary Medicines Directorate) provides advice on zoonoses and antimicrobial resistance, from the perspective of how human, animal and environmental health interact (‘One Health’). The department also supports the UK’s international influencing activity on drug resistance.
Findings
Relevance: Does the UK have a coherent strategy for using aid to address global health threats?
In this section, we assess the relevance of the government’s approach to global health threats preparedness. We look at whether an appropriate and balanced strategy and programme portfolio were developed, based on learning and experience from the Ebola crisis and other evidence. We include consideration of whether DFID’s existing health programming has been sufficiently adapted to meet the imperative to tackle global health threats. Finally, we look at how well aligned the UK’s approach is with other donors and multilateral organisations active in this field.
In response to the Ebola crisis, the UK moved quickly to develop a coherent strategy for addressing global health threats
The inadequacy of the international response to the Ebola outbreak was a key driver behind the UK’s decision to scale up its investment in global health threats preparedness. From 2014 onwards, there was an effective cross-government effort to marshal the learning from the Ebola crisis, alongside evidence of the growing threat of drug resistance. This was rapidly translated into a set of policy proposals to reduce the impact of global health threats and crises, covering WHO reform, improved surveillance and access to medicines, tackling antimicrobial resistance, and a rapid response team.
By mid-2015, the UK had produced a coherent framework for action, Stronger, Smarter, Swifter. We found that the framework represents a relevant and balanced strategy for addressing the system weaknesses exposed by the Ebola crisis, as well as the ongoing challenge of drug resistance. It is also consistent with the high-level commitments of the 2015 UK aid strategy and the 2015 National Security Strategy and Strategic Defence and Security Review to strengthening the international response to health crises (including strengthening multilateral institutions, investing in science and technology and rapid response). The October 2017 Humanitarian Reform Policy also emphasises the importance of strengthening country health systems as part of health crisis prevention and response.
A number of success factors that supported the rapid development of the strategy for tackling global health threats were identified by the government and external stakeholders consulted for this review. These include:
- strong political leadership, including from the Cabinet Office minister and from the Prime Minister’s office
- the real-time nature of the review of the Ebola crisis, bringing added urgency
- the leveraging of external expertise
- rapid access to quality technical inputs at departmental level.
The framework’s focus on enhancing prevention and detection of, and response to, global health threats reflects the priority areas for intervention identified by external experts consulted for this review as well as the wider scientific literature (see Box 8).
Box 8: Evidence supporting the Stronger, Smarter, Swifter framework
Stronger
- The framework’s priorities to strengthen WHO capacity and leadership, and to reinvigorate commitment to the International Health Regulations on disease surveillance and reporting (see Box 4), are widely cited in the literature as necessary for improving the international response to global health threats.
- The focus on strengthening national health systems is supported by evidence on the need for disease-specific interventions to be complemented with broader health systems strengthening in order to better prepare countries for outbreaks and increase their resilience.
Smarter
- The Smarter theme of activity reflects an identified need for more effective vaccines, diagnostics and medicines for epidemic diseases, which can be brought onstream more rapidly during a crisis.
- The theme’s focus on international advocacy efforts is backed up by strong evidence (including the O’Neill review). Global commitments are necessary to combat antimicrobial resistance and establish new systems of surveillance in developing countries, due to the global scale and reach of the problem of resistance to antibiotics.
Swifter
- Swifter commitments to deploying public health and epidemiological expertise are supported by a strong consensus within the literature on the need for more effective rapid response mechanisms.
- The framework’s objective to leverage increased financial resources more rapidly during an outbreak reflects a clear recommendation from Ebola lesson-learning exercises.
We share the concern of some government stakeholders who questioned whether the framework gives sufficient attention to the specific challenges of addressing outbreaks in fragile or conflict affected settings, where the risk of epidemics is increased. DFID suggested that there is greater scope for learning from its humanitarian response operations, to inform both the overall strategy and the delivery of particular programmes such as the deployment of the UK Public Health Rapid Support Team.
The UK aid strategy pledges to make better use of the diverse expertise available across government. In the case of Stronger, Smarter, Swifter, responsibilities were allocated between the two main delivery departments, DFID and the Department of Health. This was largely based on existing departmental strengths, while also demonstrating the capability of these departments to adapt their activities in response to the lessons learnt from Ebola. For example, under Smarter, the Department of Health expanded its existing focus on vaccine development and drug resistance, while DFID built on its strengths in developing diagnostic tools and country implementation research. However, DFID also adapted its research to focus more on epidemic diseases, provide flexible research funding (to help respond to new emergencies) and include social science perspectives.
While there is a rational division of responsibilities between these two main departments, it is less clear whether and how other government departments are expected to contribute. For instance, the framework does not mention a range of relevant cross-government ODA-funded research programmes, such as the £1.5 billion Global Challenges Research Fund (GCRF) and the £735 million Newton Fund, both of which are managed by the Department for Business, Energy and Industrial Strategy and include research on infectious diseases, health systems strengthening and antimicrobial resistance (see Annex 3).
The lack of links to other relevant cross-government research efforts constitutes a gap in the Stronger, Smarter, Swifter strategy, identified by both government experts and the review team. The framework’s research priorities are narrowly focused on the development of new products (for example vaccines for epidemic diseases). The framework neglects the need identified during the Ebola crisis for better social science-based research, for example aimed at understanding the social and cultural aspects of how epidemics spread, or how to strengthen health systems in such contexts.
DFID and the Department of Health developed a relevant and proportionate set of centrally managed programmes to strengthen the response to global health threats
Over the course of 2016, the Department of Health and DFID put together a portfolio of new and adapted centrally managed programmes, which we found to closely reflect the priorities of Stronger, Smarter, Swifter (see Figure 2 and Annex 2).
Each intervention within the portfolio responds to a distinct objective within the framework, while contributing to a set of coherent and mutually supportive approaches overall. For example, large scale investments in new vaccines are part of the Smarter response to diseases with epidemic potential. But these investments also support the fight against drug resistance, given the role that immunisation plays in lowering the incidence of initial infection and hence the need for treatment with antibiotics. Programmes funded under Stronger demonstrate a complementary, multi-level response to the framework’s commitments to strengthening the disease preparedness of health systems. These include:
- influencing WHO reforms at the global level (through the UK’s Core Voluntary Contribution and performance agreement)
- driving regional WHO reform (through the Tackling Deadly Diseases in Africa Programme)
- country systems work (through the International Health Regulations strengthening programme and relevant DFID bilateral health programmes).
The Department of Health and DFID have drawn on relevant evidence to support the case for individual programmes within the portfolio. Within programme business cases, there is further reference to the lessons learnt from Ebola and the scientific literature, as well as expert partner inputs and project-specific research. For example:
- DFID undertook a survey of health advisors to better understand the WHO’s performance at the country level.
- For the Tackling Deadly Diseases in Africa Programme, DFID drew on the WHO Joint External Evaluation assessments of how well countries adhered to the International Health Regulations to determine where to focus its support.
- In Sierra Leone, the need to strengthen the health workforce was evidenced through a survey that identified the number of active health workers relative to the total payroll.
While there is a significant threat posed by new epidemic outbreaks and drug resistance, there is also a disease burden from more long-standing health problems such as HIV/AIDS, tuberculosis and malaria. Importantly, we found that the portfolio of new and refocused global health threats programmes has not resulted in reductions in UK spending on other global health priorities. The government has maintained its significant expenditure on tackling more established diseases since the Ebola crisis, for example through its contributions to the Global Fund and Gavi. We therefore agree with the government and external stakeholders interviewed that the current focus and level of expenditure on global health threats is broadly appropriate.
At the time of this review, the Department of Health (with DFID’s input) was also in the process of developing logic models and theories of change for the framework. These should be helpful for internal coordination and communicating the framework to external stakeholders.
The role of country health systems strengthening needs more emphasis across the Stronger, Smarter, Swifter framework and in centrally managed programmes
A number of the expert stakeholders we consulted, as well as some DFID representatives, were concerned that the new focus on epidemic threats should not come at the expense of health systems strengthening in partner countries (a key lesson from the Ebola crisis). We therefore looked at the prominence given to health systems strengthening within the framework as a whole, within centrally managed programmes and in DFID’s bilateral health programmes.
Positively, the framework includes a number of references to building country health systems within the Stronger theme of activity. However, the framework views health systems strengthening from the narrow perspective of meeting the International Health Regulations and improving disease surveillance, rather than taking a broader approach drawing on the WHO’s ‘six building blocks of an effective health system’. Moreover, the framework does not articulate in enough depth how the strengthening of health systems is valuable across all of the themes of Stronger, Smarter, Swifter. Health experts we consulted stressed that it is important to integrate disease preparedness activities (such as on antimicrobial resistance) within longer-term approaches to building sustainable health systems, wherever possible.
It follows that we found varying emphasis on sustainable health systems strengthening across the portfolio of centrally managed programmes. System strengthening is a key focus of the International Health Regulations Strengthening and Tackling Deadly Diseases in Africa programmes. By contrast, the business case for the Fleming Fund does not articulate its potential contribution to the strategic objective of health systems strengthening, although aspects are referred to in relation to programme delivery. In Burma, we found that the alignment between the Fleming Fund and broader efforts to strengthen the country’s health systems could have been stronger.
We found that Gavi’s health systems strengthening grants are channelled in many recipient countries through intermediary bodies, including UNICEF, and then to civil society organisations, rather than through government health systems. This reflects pressure to ensure accountability for donor funding, but may also miss a potential opportunity to strengthen national health systems.
DFID’s country-level health programmes are evolving in line with global health security priorities, although there is much more to do
In DFID’s plans and programmes at the country level, we found more of a mixed picture on the extent to which global health security priorities had been integrated. Only six out of 17 DFID operational plans developed between 2014 and 2016 referred to tackling global health threats, and only nine out of 24 DFID countries with health programmes had integrated global health threats activities into them. More positively, ten operational plans demonstrated an increased level of prioritisation of health systems strengthening over the period.
We selected four countries for in-depth review among the nine that had programmes with relevant global health threats activities: Burma, Ethiopia, Nigeria and Sierra Leone. In these countries, we found varying degrees of success in integrating objectives and activities related to global health threats, from specific activities such as enhancing surveillance systems and emergency response capabilities through to sustainable health systems strengthening.
Perhaps not surprisingly, given the Ebola experience there, bilateral programmes in Sierra Leone were most relevant to health threat preparedness (see Box 9). Based on our programme reviews and the survey of DFID health advisors, the Provincial Health and Nutrition Programme in Pakistan (2012-18) appears to be a more typical example of how global health threats priorities have been incorporated within bilateral health programmes. The programme includes a stand-alone project, delivered by Public Health England, on strengthening disease surveillance and compliance with the International Health Regulations. Outside of this specific project, we found a general lack of linkages between country-level programmes and the Stronger, Smarter, Swifter framework.
Box 9: Health programme alignment with Stronger, Smarter, Swifter in Sierra Leone
The DFID bilateral programme Resilient Zero (2016-17) aimed to prevent further Ebola transmission and to enhance preparedness against future outbreaks. This was to be achieved through developing stronger surveillance of diseases (working with WHO), smarter detection (through new laboratories and diagnostic tests supported and implemented by Public Health England) and a swifter response (through funding a fleet of vehicles and a deployable isolation treatment facility, working with the UK military).
The longer-term Saving Lives programme (2016-21) has a dual focus on reducing maternal and child mortality and strengthening resilience to infectious disease outbreaks. While primarily targeting maternal health, the programme also pursues a health systems strengthening approach, which largely reflects the WHO building blocks. DFID Sierra Leone and consortium partners are working with the government of Sierra Leone to:
- strengthen the health workforce, including community health workers
- improve health information and data sharing (including building on the surveillance and districtlevel
- capacity developed by Resilient Zero)
- improve access to medicines
- support national health strategy and planning.
Among the DFID country health programmes we reviewed, we observed few examples that were focused on tackling drug resistance directly. The exception was in Burma, where we saw programmes aimed at detecting and treating drug-resistant malaria and multi-drug-resistant tuberculosis, in response to evidence of the emerging prevalence of certain types of drug resistance across East Asia.
In many countries, the private sector (ranging from small informal drugs outlets to private sector hospitals) plays a large and growing role in health care delivery. However, in our sample of country programmes, we found strategies for private sector engagement at country level to be weak. The exception was Burma, where programmes engaged with private sector drug manufacturers, distributors and vendors to help phase out less effective anti-malarial therapies and to introduce simple diagnostic tests as part of the efforts to tackle drug resistance.
In our interviews, DFID advisors showed a good understanding of the link between disease preparedness and building more resilient health systems. But in the bilateral country programmes on global health threats that we reviewed, we found that health systems strengthening was an implicit rather than explicit objective. DFID country office staff told us that there is a need for guidance on how to maximise synergies between global health security programmes and health systems strengthening. Some government stakeholders and other donor representatives articulated a need to move from specific disease-focused approaches towards direct financial support for building government health systems and health services.
DFID was finalising a ‘UK position paper on strengthening health systems’ at the time of this review. The draft reviewed by the ICAI team included helpful explanations of the links between global health security and health systems strengthening (including the WHO’s building blocks). Publishing this will provide useful guidance for integrating aspects of health systems strengthening within both centrally managed and country-level programming.
The UK’s strategy adds value to international efforts by filling gaps and ensuring complementarity
UK programmes and influencing activities complement the efforts of other donors and international organisations by supporting the International Health Regulations, the WHO Research and Development Blueprint (which identifies priority infectious diseases to guide research and development activity) and the WHO Global Action Plan on Antimicrobial Resistance.
While a number of donors (including the US, Germany and Japan) are supportive of WHO reform, the UK is perceived as a leader in this area. Its linking of performance targets to its voluntary contributions is ground-breaking, with the WHO acknowledging that this is helping to focus reform efforts internally. Public Health England’s work supporting the International Health Regulations, and the UK Public Health Rapid Support Team, are embedded within the WHO’s systems, thereby helping to strengthen these systems and avoid duplication. At the country level, we found that DFID was often playing a coordinating role, building on its long-standing country presence and established forums involving partner governments and other donors. In Sierra Leone and Nigeria, DFID was supporting country health plans and facilitating strategic alignment across bilateral donors, UN agencies,nongovernmental organisations and these governments around strengthening country health systems.
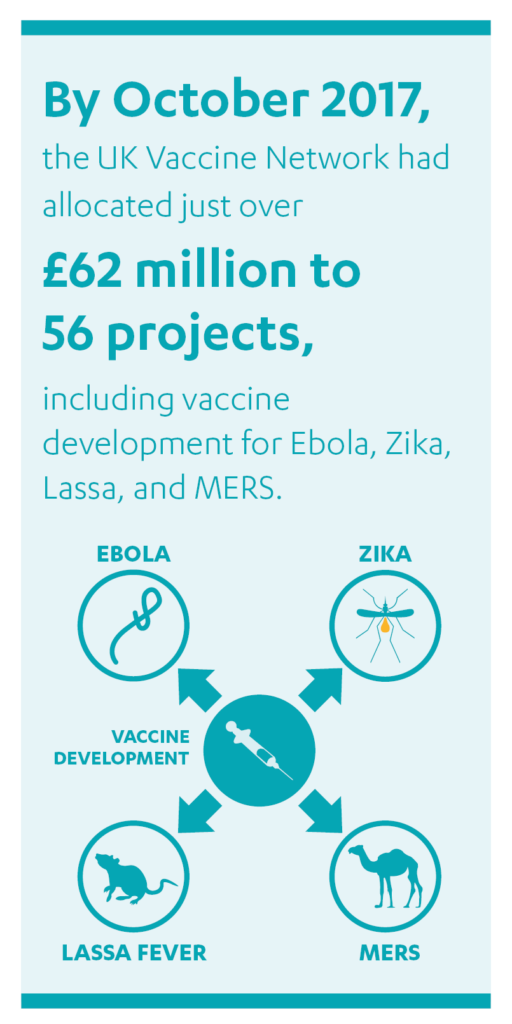
The UK government’s investments in vaccines are complementing rather than competing with the private and philanthropic sectors. The UK Vaccine Network avoids duplication by targeting vaccines for uncommon diseases, where there is less private sector investment. The programme also has direct representation from the private sector among its membership. Gavi, the Vaccine Alliance, has placed greater emphasis in recent years on mobilising financial and other contributions from the private sector.
The UK is also adding value to the international effort by filling gaps in funding. For instance, the WHO Africa Regional Office told us that the UK is the only bilateral donor supporting them directly, despite general recognition that the WHO regional level needs strengthening. The UK-supported Contingency Fund for Emergencies fills another gap: while other emergency funds are coming onstream to support more severe and widespread disease outbreaks, this is the only international funding mechanism aimed at immediate response (within the first three months) to smaller-scale disease outbreaks. In support of this, we found evidence of early mapping of donor activities during the programme design phase of DFID and Department of Health programmes.
The UK faces an increasingly difficult challenge to keep pace with an evolving international landscape
The UK was an early mover in responding to global health threats, with a high risk appetite. Ensuring that the UK’s strategy and programmes continue to align with other donors and the private sector is an increasing challenge. There are new initiatives and increased activity from the World Bank, the African Union and the Asian Development Bank. Bilateral donors such as China and Japan and philanthropic organisations such as the Bill & Melinda Gates Foundation are also increasingly engaged. This presents an opportunity for the UK, but also a coordination challenge.
Increased cooperation and coordination between the UK’s approaches and those of other donors could reduce overlap and enhance overall impact. This could include collaboration on country health systems strengthening work, for example with Germany and the Bill & Melinda Gates Foundation, or with the World Bank on investments in surveillance systems and financing emergency response.
Closer cooperation between the UK Vaccine Network and the Coalition for Epidemic Preparedness Innovations would also be beneficial. The Coalition was established approximately 18 months after the UK Vaccine Network. The two initiatives have a common goal, and focus on supporting overlapping sections of the vaccines pipeline, particularly the mid-stage development of vaccines for epidemic diseases.
We found that existing mechanisms for coordination with external donors and the philanthropic and private sectors around global health threats preparedness are underdeveloped, beyond high-level meetings such as the G7, G20 and World Health Assembly. UK support for new structures such as the WHO’s Global Coordination Mechanism for Research and Development (linked to the WHO Research and Development Blueprint) and the Global Antimicrobial Resistance Research and Development Hub (see 4.62) represent a step in the right direction for achieving Smarter objectives. However, strong coordination mechanisms are lacking in other critical areas such as health systems strengthening (Stronger) and financing emergency response (Swifter).
Compounding this, the UK government has never published the Stronger, Smarter, Swifter strategic framework, nor provided comprehensive information on its portfolio of global health threats interventions or how responsibilities for these are divided between different departments externally.
Increased communication and openness would have helped partners to better align their spending with the UK government’s priorities and to avoid overlap. The Department of Health and DFID acknowledged that the development of a revised, more outward-facing strategy is required to ensure its ongoing relevance and coherence, particularly with external initiatives.
Conclusions on relevance
The UK moved quickly to diagnose the challenges relating to global health threats, based on evidence from the Ebola crisis and the emerging risk of drug resistance. The Department of Health and DFID responded with a relevant and well-balanced Stronger, Smarter, Swifter strategic framework underpinning a portfolio of interventions. Each major programme is supported by evidence of a strong strategic rationale.
The importance of social science-based research and health systems strengthening could be more clearly laid out within the framework. DFID country health programmes are evolving in line with the framework, but there is a need for global health security interventions in general to adopt a more explicit cross-programme focus on health systems strengthening. Links with DFID’s humanitarian policies could be strengthened, including approaches to responding to new outbreaks in fragile or conflict-affected settings.
Changes in the wider environment since the framework was developed highlight the need for a strategy review and refresh. With a number of actors entering or scaling up their activity in this area, it has become increasingly clear that the UK government needs to communicate and promote its strategy more clearly to other relevant actors and strengthen coordination mechanisms. Not doing so limits the government’s influencing capability and reduces the potential for other donors to align their activities and spending to the UK effort.
Overall, we have awarded the UK government’s global health threats agenda a green-amber for relevance. This recognises the considerable achievement in the wake of the Ebola crisis of developing a coherent framework for addressing global health threats, as well as a relevant portfolio of centrally managed programmes and influencing activities. However, there is a need to update its strategy in line with recent external developments, to clarify and strengthen the links between global health security and health systems strengthening, and to disseminate its strategy externally.
Effectiveness: Is the emerging aid portfolio a potentially effective response to global health threats?
In this section, we examine the effectiveness of the UK aid portfolio on global health threats. We take a separate look at each of the three themes of the portfolio, investigating in turn the performance and potential of programmes in our sample under Stronger, Smarter and Swifter. Given the early stage of delivery, with programmes largely covering the period 2016-21, this is based on an assessment of the potential effectiveness of programming and influencing work, as indicated by their plans and initial progress. We also review the extent to which wider ODA-funded research is being leveraged to support global health threats preparedness. Finally, we look at the effectiveness of the government’s coordination efforts.
Under the Stronger theme, UK interventions are helping to improve the responsiveness of the international system to global health threats
The main priority under Stronger is at the international level: encouraging WHO reform. The UK has used an appropriate combination of influence with the WHO and with other stakeholders, funding linked to performance targets and the development of a supportive relationship with the WHO to encourage improvements. Critically, the WHO’s leadership is supportive of the reforms agreed with the UK, and sees them as aligned with the organisation’s own ambitions.
We found that the UK has been successful in convening support for WHO reform from other major donors, including the US, Germany and Norway. This has been facilitated by the UK holding direct discussions, including through the donor group Friends of the WHO Health Emergencies Programme in Geneva. Other bilateral donors spoke positively of the UK’s leadership role and its influence. One donor representative noted that “the UK is clearly listened to by the WHO” and added that the UK’s performance agreement had helped focus the WHO conversation about reform.
The UK’s efforts have been influential in encouraging improvements in management and accountability within the WHO, as well as in increasing the organisation’s responsiveness to disease outbreaks. DFID’s first annual assessment (completed in mid-2017) of the UK’s £58 million Core Voluntary Contribution confirmed that the WHO was meeting all of its critical performance indicators and in several areas was exceeding expectations, including in risk management, financial management, transparency and working in partnerships (for example with Gavi, the Vaccine Alliance). Positive progress was also evidenced by the WHO’s response to the Zika virus (Box 10).
Box 10: Improvements since Ebola: an effective response to the Zika outbreak
On 1 February 2016, WHO convened an expert emergency committee to assess the Zika virus outbreak in the Americas and the threat it posed. The same day, it declared a Public Health Emergency of International Concern. A comprehensive strategic response plan followed two weeks later. The Contingency Fund for Emergencies was triggered and funds disbursed within 24 hours of the declaration, in accordance with the UK’s performance agreement target. A full incident management structure was set up at the WHO headquarters and all regional offices, and training and public awareness activities were carried out. The Zika appeal response was slow initially, with contributions from other donors only coming through six weeks into the outbreak. The WHO’s Contingency Fund filled the gap, allowing donors time to judge the potential impact of the outbreak and consider how to respond.
The UK government acknowledged that the WHO still needs to make significant progress, but that it is “pointing in the right direction”. The factors behind the UK’s success in influencing WHO reform include a coherent shared vision and an effective joint approach between the Department of Health and DFID to help maximise influence on WHO reform, an annual UK-WHO strategic dialogue, and the leadership of the UK’s Chief Medical Officer.
The UK government’s influencing activities extend to the regional and national levels. The Tackling Deadly Diseases in Africa Programme includes an action framework between the UK and the WHO Africa Regional Office. The framework details how the two will work together to improve health security and universal health coverage in Africa, and create a responsive and results-driven WHO secretariat. DFID’s prominent role has also helped influence the Bill & Melinda Gates Foundation to provide support to the WHO Africa Regional Office.
We also found evidence of limits to the UK’s influence. Only modest progress was made on leveraging additional funding to support the WHO’s Health Emergencies Programme (see 4.78). Strengthening the accountability of WHO regional and country offices (outside of the WHO Africa Regional Office), and addressing their capacity constraints, have proved challenging.
Positively, the UK has reacted to these limitations by attaching new performance indicators to the Core Voluntary Contribution for 2017-18. These include improving the quality of the WHO’s country representatives and making progress on replenishing the Contingency Fund for Emergencies.
DFID recognised that ultimately it is up to the WHO to demonstrate through continued improvements why donors should support the organisation. However, DFID and other bilateral donors also acknowledged that they could do more to reach out beyond the like-minded member states that they currently work with in Geneva, in order to help influence a broader set of donors to commit funding to WHO reform. We also found that some DFID country offices could interact more with the WHO, in order to help encourage quick wins and improve the WHO’s accountability at this level.
UK support for implementation of the International Health Regulations is likely to have a positive impact
Another priority under the Stronger theme is the £16 million International Health Regulations Strengthening programme, led by Public Health England. We judge that this programme is likely to make an effective contribution towards its target countries meeting health regulation requirements. The programme is underpinned by a strong evidence base, the prior experience of Public Health England in supporting country compliance with the regulations and positive engagement with country governments. There is also evidence of a strong partnership between the programme and the Tackling Deadly Diseases in Africa Programme. This should help to ensure a mutually supportive approach to strengthening health systems in the region.
At the time of our review, Public Health England had completed scoping missions to appraise the requirements of each target country, and received positive responses to its implementation plans from partner governments. This should also help ensure that the programme has a stronger and more sustainable impact on country health systems. Box 11 summarises the results of the Nigerian scoping mission.
Box 11: Public Health England’s scoping mission to Nigeria
Nigeria, Africa’s most populous country with more than 190 million inhabitants, is one of five countries that took part in the scoping phase of Public Health England’s International Health Regulations Strengthening programme. Nigeria has some of the world’s highest levels of tuberculosis and malaria, and a number of zoonotic diseases with epidemic potential. West Africa has a long tradition of regional migration, and communities straddle international borders. A stronger, more resilient Nigerian health system, better able to contain epidemics, would therefore have positive effects beyond its borders.
Public Health England’s scoping mission to Nigeria led the agency to conclude that there is strong political will, in-country leadership and donor interest in place, suggesting that the country is well placed to achieve rapid and significant improvements in its health systems. Based on this conclusion, Public Health England will support the Nigerian government in undergoing a full health systems evaluation (WHO’s Joint External Evaluation) and will help develop and implement an action plan to address weaknesses exposed by this evaluation.
Despite this positive progress, we observed room for improvement in coordinating the work of Public Health England, DFID’s bilateral health programming and the Fleming Fund, to help countries meet the International Health Regulations. DFID suggested that the WHO’s Joint External Evaluation process and country action plans (once complete) should help to improve coordination by providing a common set of priorities to work towards.
DFID’s country programmes with a focus on global health threats are helping to strengthen the capacity of national health systems, although more could be done
The Stronger theme includes an objective for countries to develop “resilient, responsive and accountable health systems, including surveillance”, and to make progress towards meeting International Health Regulation obligations. Alongside support from the Fleming Fund, the UK government’s contribution is delivered primarily through bilateral health systems strengthening efforts.
We concluded that each of the DFID country programmes we reviewed (in Burma, Nigeria, Pakistan and Sierra Leone – see Figure 3) is beginning to make an effective contribution to global health threats preparedness. We base our conclusion on the appropriateness of programme designs, the strong overall performance of DFID’s health programmes, and emerging evidence of positive contributions towards the development of well-functioning health systems. We also saw evidence that DFID is influential in its relationships at country level, with other bilateral donors, with multilateral partners and with country governments.
The work of DFID’s £38 million Resilient Zero programme in Sierra Leone to help build an effective surveillance and response system, in partnership with the WHO, Public Health England and others, provides an illustrative example of an effective contribution to global health threats preparedness (see Box 12).
Box 12: Case study – building effective surveillance in Sierra Leone
As part of Resilient Zero, the UK contributed £7.7 million to the WHO Sierra Leone office to improve systems for the detection of diseases with epidemic potential. This helped revitalise an integrated disease surveillance and response system and supported training for community health workers to conduct community-based surveillance. Resilient Zero supported continuity by building on the operational support that DFID had provided during the Ebola outbreak, for example to district health management teams.
Through this support, Sierra Leone has built up what one external stakeholder called an “extremely well-functioning detection system”. All health facilities provide weekly reports on 26 different diseases, and these are aggregated into a national report, which is discussed in weekly meetings with the government and health partners. The Joint External Evaluation of Sierra Leone’s progress towards compliance with the International Health Regulations judged Sierra Leone to have “robust” systems in place.
Reporting rates across districts are now in excess of 90%. Numerous alerts have been reported over the last two years, covering diseases from measles and monkey pox to Ebola. This surveillance structure proved useful following the August 2017 mudslide in Freetown by supporting a coordinated and responsive approach to suspected cholera cases (including deployment of the UK Public Health Rapid Support Team).
While, as previously noted, health systems strengthening was not an explicit objective of the country programmes reviewed, all programmes included at least some activities that have made a positive contribution towards the WHO’s building blocks of a well-functioning health system. For example, the £150 million Saving Lives programme in Sierra Leone and the £118 million Three Millennium Development Goal (3MDG) Fund programme in Burma were covering most or all of the building blocks of an effective health systems. Specific examples of the contributions of DFID’s bilateral programmes to building responsive and resilient health systems are included in Annex 4.
Nonetheless, DFID’s country health programmes have only recently adapted to address global health security priorities. We found that the effectiveness and sustainability of programmes could be increased by moving towards a more explicit focus on health systems strengthening, alongside their existing focus on specific health issues (such as maternal health) or single diseases (such as malaria).
This shift will necessarily involve working more closely with governments, and often also with private sector health care providers. However, DFID faces tensions in moving towards this model of health systems strengthening, given existing approaches of channelling ODA health funds through multilateral and civil society organisations rather than through direct budget support.
We identified a number of good examples of DFID programmes working more closely with partner governments (but without providing direct budget support). These centre on providing different forms of technical assistance to ministries of health, and promoting institutional capacity building:
- In Sierra Leone, Saving Lives has commissioned external organisations to provide direct technical assistance to the Ministry of Health, including the work of the Clinton Health Access Initiative in developing a Human Resources for Health strategy. DFID also sponsors a health advisor to work for the country’s Chief Medical Officer. More broadly, health donors meet regularly as part of government-chaired committees.
- In Burma, the 3MDG Fund is supporting sub-national capacity building at community and township levels in order to help improve health management capabilities and accountability.
- In Nigeria, a Health Funders Forum provides an effective interface with government (for example all programme work plans are developed in consultation with government partners).
The UK government could provide stronger international policy leadership on country health systems strengthening, although new initiatives are underway
We did not see strong evidence of UK achievements in global policy leadership on country health systems strengthening during the review period. For example, while DFID began drafting a UK position paper on strengthening health systems in 2015, with the intention of sharing this with other bilateral donors to help influence policy, the paper has not yet received ministerial sign-off or been disseminated.
DFID recognises the need for greater progress in this area. It aims to launch the position paper, together with a new DFID programme, ‘Making Country Health Systems Stronger’, in early 2018. This programme will seek to encourage different departments within the WHO, including the Health Emergencies Programme, to focus on strengthening health systems as a whole. It will be complemented by the incorporation of a new indicator to encourage health systems strengthening as part of the International Health Regulations.
Under the Smarter theme, UK programmes and influence are likely to improve the detection of antimicrobial resistance
Several stakeholders highlighted the important role of the UK government, and the commitment of the Chief Medical Officer in particular, in pushing the prioritisation of drug resistance within the WHO. One bilateral donor described the UK as at the “very, very forefront” of driving WHO action around antimicrobial resistance.
Working with other like-minded donors, and leveraging the influential O’Neill review on antimicrobial resistance, the UK government successfully lobbied for the adoption of international political commitments on tackling antimicrobial resistance. These include the endorsement by the World Health Assembly of the Global Action Plan on Antimicrobial Resistance (2015), the adoption by the UN General Assembly of the Political Declaration of the High-Level Meeting on Antimicrobial Resistance (2016), and the establishment of the Global Antimicrobial Resistance Research and Development Hub to coordinate investment across G20 members and non-government donors (2017).
We judge the £265 million Fleming Fund to have strong potential to contribute to effective country surveillance and detection of drug resistance. The contractors hired by the Department for Health to manage the Fund have undertaken an extended scoping phase to refine programme activities prior to implementation, including mapping the activities of other donors. In parallel with this, the Fleming Fund has supported the production of country-level antimicrobial resistance action plans, which should help guide implementation on the ground. Positively, this initiative was coordinated through the WHO.
In support of sustainability, the Fleming Fund will aim to leverage other funding, using evidence generated from its own evaluations to help justify investments. There are also plans to create an international network of Fleming Fund Fellows: health practitioners from different disciplines and sectors who will receive professional development support and form ongoing communities of practice.
We found that the Fleming Fund experienced challenges during its inception phase. The Department of Health, which was new to managing international development funding, initially lacked experience in the legal, procurement and assurance aspects of ODA, along with an associated low appetite for risk and internal staffing constraints. The implementation plan for the largest element of the Fund – support for country-level surveillance systems – was originally expected to be signed off in the summer of 2017, but this had not happened by the end of the year. The Department of Health has acknowledged the need for more senior-level inputs to help allay procurement risk concerns and has now strengthened its Global Health Security Team.
Fleming Fund reviews of country requirements do not always clearly articulate the nature of the support required, leading to missed opportunities for working in a joined-up way with national governments and other donors. For instance, in its early engagement with Burma on antimicrobial resistance, the Fleming Fund could have worked more closely with the DFID Burma office and Public Health England experts to get a better understanding of the country context. It could have aligned the phase-in of its programme more closely with the efforts of other actors, and placed a stronger emphasis on helping the Burmese government improve its own technical capacity on antimicrobial resistance.
UK programmes are likely to help plug gaps in the availability of vaccines and diagnostics and in research for epidemic diseases
The Smarter strategy commits to addressing gaps in the availability of vaccines, drugs and diagnostic tools for diseasesof epidemic potential. The programmes we reviewed – the UK Vaccine Network and DFID’s Ross Fund research portfolio – harness significant capacity and expertise from different sectors and organisations and demonstrate strong potential to deliver on this commitment. The programmes have demonstrated positive progress to date, including influence over global policy.
The initial work of the £110 million UK Vaccine Network focused on identifying priority diseases based upon the level of threat that they posed. By the end of October 2017, just over £62 million had been allocated to 56 projects on a competitive basis. The projects include developing new vaccines for diseases such as Zika and Lassa fever, supporting clinical trials to bring these vaccines to market and establishing a £10 million Centre for Innovative Vaccine Manufacturing. Collaboration between the Department of Health and the UK’s research councils, who manage the funding competitions, was key to the successful allocation of the funding.
Projects funded under DFID’s Ross Fund research portfolio for epidemic diseases have strong potential to be effective, building on previous successful projects within DFID and on strong partnerships with the WHO and the Wellcome Trust:
- Support for the development of the WHO Research and Development Blueprint for action to prevent epidemics (£6 million) is a longer-term strategy to help establish an international list of priority diseases for investment and a Global Coordination Mechanism for Research and Development. We found that the WHO welcomed the UK government’s role and called for increased efforts from the UK to help align other donors, research organisations and pharmaceutical companies around the Blueprint’s priorities for investment.
- The DFID-Wellcome Trust partnership (£19 million) funded a rapid research call for Zika, showing how the Ross Fund can be used flexibly in response to new outbreaks or health emergencies. A memorandum of understanding between DFID and the Wellcome Trust has since been finalised. Further joint calls for research proposals were being planned at the time of this review.
- The £30 million Foundation for Innovative New Diagnostics, which is supporting the development of new diagnostic tools for malaria, sleeping sickness and tuberculosis, is progressing well.
Longer timeframes are required for Smarter investments to deliver on the aims of the framework
The three-to-five year timescale of the global health security programmes, once inception and scoping phases are taken into account, is relatively short for large-scale research and development projects. Without agreed programme extensions, it may be challenging to embed system-level changes, whether through the Fleming Fund or the WHO Research and Development Blueprint, and there may be insufficient time to fully develop new products and bring them to market. Achieving longer-term impact from the UK Vaccine Network’s investments (for example ensuring that its products are available in an outbreak), will be dependent upon leveraging further financing for the expensive mid-to-late stages of vaccine development. This may require the development of innovative financing mechanisms and other ways of engaging the private sector.
This challenge highlights again the importance of the government engaging other actors in the global health threats field to encourage alignment behind shared objectives and shared investments. In this case, relevant actors include the Coalition for Epidemic Preparedness Innovations, donors investing in products for epidemic diseases, and pharmaceutical companies working on vaccine production and antimicrobial resistance. There may be interesting lessons to be learnt from the Department of Health’s own domestic experience of incentivising the private sector to produce new antibiotics.
Under the Swifter theme, UK programmes have supported a more rapid response to new outbreaks
The UK’s £6.2 million contribution to the WHO’s Contingency Fund for Emergencies was effective in achieving its immediate goals. Over the course of 2016-17, the WHO dispersed funding in response to new outbreaks in a timely manner (see Box 10). It also improved its systems, including establishing an international oversight advisory committee.
The UK Public Health Rapid Support Team is an equal partnership between Public Health England and the London School of Hygiene and Tropical Medicine. We identified a number of strengths to the model, including its globally recognised expertise, flexibility to deploy swiftly in different contexts, strong coordination with the WHO, and focus on country research and capacity building. Building on this foundation, during 2017 experts from the UK Public Health Rapid Support Team were successfully deployed to Ethiopia, Nigeria and Sierra Leone. This helped to strengthen surveillance and case management, supported the WHO country teams, and developed local capacity to manage disease outbreaks. The team has also contributed to broader WHO reform priorities, through providing technical support for the improved coordination of rapid response teams across different countries.
Figure 4: UK Public Health Rapid Support Team deployments
| Ethiopia | Nigeria | Sierra Leone |
|---|---|---|
| April - May 2017 | May - June 2017 | August - September 2017 |
| Deployed to support the WHO response to an acute outbreak of cholera. | Deployed through WHO to address a new outbreak of meningococcal meningitis. | Deployed bilaterally as a preventative measure following flooding and landslides. |
We found that the UK Public Health Rapid Support Team would benefit from a clearer set of performance targets to help guide delivery, and to enable a more objective evaluation of its effectiveness and achievements during different health emergencies. Evidence of these in its reports on country deployments is currently largely anecdotal.
Gavi, the Vaccine Alliance, is now better placed to contribute to strengthening the response to future disease outbreaks, following recent improvements in accountability at the country level. These include increasing the number of country managers at its Geneva headquarters and focusing health systems grants on strengthening immunisation systems. In Burma, we also saw evidence of Gavi helping the government to strengthen its financial/grant management capabilities.
The UK, as the largest donor to Gavi, has been highly influential in driving these efforts. Gavi staff describe the UK as “the most engaged donor”. However, strategic stakeholders would like to see greater engagement from DFID country offices with Gavi grants at the local level, to improve local accountability and alignment of health systems strengthening activities.
Gavi has funded stockpiles of vaccines for yellow fever, cholera and meningitis to ensure a more rapid response in the event of new outbreaks. In 2016, Gavi also launched a US$5 million advance purchase commitment to support the development of an Ebola vaccine, following successful clinical trials funded by the Wellcome Trust. In Burma, health systems strengthening efforts are focused on the cold chain for vaccine distribution, enabling more remote populations to be reached.
The UK has been less successful in influencing other donors to increase their financial support for addressing new outbreaks
The UK’s strategy for improving the global capacity to respond to new outbreaks is predicated on influencing other donors to also increase their funding. The success of this influencing effort has been limited. For instance, the UK sought to increase contributions to the Contingency Fund for Emergencies, following evidence of its success (see Box 10). However, by the close of the 2016-17 programme, the Fund had attracted less than 40% of the required financing, and the WHO had not yet established a replenishment strategy (resulting in DFID adapting its performance agreement).
The UK is nonetheless well positioned to support a coordinating role between emergency response funds and the needs of partner country governments, and to continue to make the case for replenishing the Contingency Fund for Emergencies. For example, DFID advocates greater flexibility in using the larger UN Central Emergency Response Fund and better links between it and the Contingency Fund.
While the UK emphasises the importance of the WHO making the case for itself, it was also clear that across various themes of activity within Stronger, Smarter, Swifter, the WHO is highly appreciative of UK support.
Effective cross-government mechanisms have been established to share evidence of disease outbreaks and consider the government’s response
While they have yet to be tested by a crisis of the scale and severity of Ebola, the new coordination structures established across UK government departments and agencies have proved effective in sharing intelligence on new disease outbreaks and informing appropriate next steps (see Box 13).
Box 13: Effective cross-government communication of health threats intelligence
International Forward Look
After the Ebola outbreak, the different departmental chief scientific advisors recognised that they could make better use of the intelligence gathered on global health threats within different departments and agencies such as Public Health England. The Government Office for Science therefore set up the International Forward Look weekly briefing for relevant government stakeholders.
During the Zika virus outbreak, early intelligence gathered by International Forward Look was used by the government’s Scientific Advisory Group for Emergencies (SAGE) to inform its decision to accelerate the use of the DFID-Wellcome Trust partnership to fund research on the health and social impacts of the outbreak.
International Health Risks Network
The Civil Contingencies Secretariat in the Cabinet Office established the International Health Risks Network in 2016. The network’s objectives are to share information on emerging global health threats with relevant government departments and ministers (building on International Forward Look) and to facilitate a clear and flexible cross-government response plan. The network convenes a monthly meeting chaired by the Cabinet Office and publishes a monthly report on disease outbreaks and associated risks.
During the yellow fever outbreak in Central Africa in 2016, this cross-government approach enabled departments to monitor the rate of infection and its geographical spread, the key risks and the response from national governments.
Cross-government coordination could be improved to implement the framework effectively
Evidence of effective cross-government coordination at the strategic level and between programmes was mixed. We saw good examples of DFID and the Department of Health working well together on their influencing efforts, particularly on WHO reform, and as part of some programmes. DFID also shared its ODA expertise with the Department of Health, providing support for the design and procurement of the Fleming Fund. DFID has representatives on the board of the International Health Regulations Strengthening programme, and the project board of the Department of Health’s Global Antimicrobial Resistance Innovation Fund.
However, DFID and the Department of Health need to coordinate better at the strategic level. We found a lack of a shared vision and protocols on health systems strengthening activities, even though the need to coordinate implementation in this area is emphasised within Stronger, Smarter, Swifter. We also found that support for the reform and strengthening of WHO country offices tended to be provided only from DFID’s WHO Core Voluntary Contribution programme, instead of being part of a broad, consistent effort by all relevant centrally managed and DFID bilateral health programmes.
We were concerned by the lack of UK-based simulations to rehearse how central government departments would coordinate and help respond to future epidemic outbreaks overseas, including how to engage with key international partners such as the WHO. This is despite recommendations to do this in a number of reports on the lessons learnt from the Ebola crisis. Some DFID stakeholders also considered that a regular table-top exercise would be beneficial in helping to pass on institutional learning from the Ebola crisis from more long-standing staff within and between UK departments. Such exercises could learn from the biannual simulation exercise on Ebola already carried out in Sierra Leone.
ODA-funded research around global health threats could be better coordinated across government. Positively, we found that DFID has used its wider health research programmes in a flexible manner to fill specific gaps in global health threats research, alongside the more substantial Smarter investments in research and development. For example, DFID used the Research for Health in Humanitarian Crises programme to undertake research on social marketing strategies for encouraging uptake of Ebola treatment in Sierra Leone (see Annex 3).
Beyond DFID’s own health research programme, though, it was less clear how far the global health threats agenda has influenced larger ODA-funded research programmes such as the Global Challenges Research Fund (GCRF) and the Department of Health’s own Global Health Research programme. We found that some research stakeholders tended to equate global health threats research narrowly with medical research, the development of new vaccines and detection of antimicrobial resistance, rather than for example recognising the important social science research challenges raised by global health threats. The gaps in research priorities set out in Stronger, Smarter, Swifter, coupled with these misconceptions by research stakeholders, make it harder to stimulate multidisciplinary research efforts in this area.
This finding chimes with our recent ICAI review of the Global Challenges Research Fund. We recommended narrowing the Fund’s research focus onto high-priority development challenges, and placing a stronger emphasis on the potential strategic development impact. Global health threats is one such challenge that would benefit from a cross-disciplinary approach, bringing medical and social sciences together and requiring strong coordination between government. The establishment of the Strategic Coherence of Official Development Assistance-funded Research Board (SCOR) may help to address the general need for greater coordination of ODA-funded research.
We found scope for improvement in engaging other government departments in global health threats preparedness. For example, the Department for Environment, Food and Rural Affairs and its associated agencies play a valuable advisory role on integrating topics relating to agriculture, zoonotic diseases and antimicrobial resistance (the ‘One Health’ agenda) into the global health threats strategy. But we received limited information about the department’s role in developing strategy and ODA programming in this area and how it joins up with other government actors on this agenda.
Coordination challenges may reflect weaknesses within existing governance structures
A range of UK coordination mechanisms relevant to global health threats were described in section 3, including the Global Health Oversight Group, the Cabinet Office’s International Health Response Network and a number of cross-government global health research forums. While we understand that these mechanisms are still developing, and that formal accountability rests with individual departments, it remains unclear how they interact. It is also unclear whether these mechanisms are performing effectively as a whole and supporting coordination and coherence across the global health threats portfolio. More specifically:
- UK government stakeholders we talked to suggested that the membership of the Global Health Oversight Group, chaired by the director generals of DFID and the Department of Health, is too limited, and that the group is not performing as effectively as it could in leading global health threats policy.
- Individual Department of Health programmes report formally to a global health security programme board. This has some DFID representation, but DFID health programmes are not part of this governance structure, limiting the potential for programme synergies across the global health security portfolio.
The framework for Stronger emphasises the importance of coordinating country-level work in support of the International Health Regulations and broader health systems strengthening. We consider that DFID country offices are best positioned to perform this role, coordinating programmes around common priorities agreed with country governments and other partners. However, we found that closer coordination of a growing portfolio of centrally managed and country programmes related to global health security, alongside an expanded health systems advocacy role with country governments and other investors, is posing a capacity challenge for DFID health advisors.
Conclusions on effectiveness
The UK has a portfolio of potentially impactful programmes. Centrally managed programmes have generally made positive progress to date, despite delays to some programmes during their inception phases, across the Stronger, Smarter, Swifter framework. DFID country health programmes are generally performing well and are making some positive contributions towards strengthening surveillance and country health systems. Cross-government efforts to develop improved coordination mechanisms for assessing and responding to data on disease outbreaks have been effective.
The UK has demonstrated leadership on global health threats policy. It has been persuasive in encouraging WHO reform and global political commitments on antimicrobial resistance, but less successful in influencing other donors’ investment choices.
A key lesson from the Ebola crisis was the need to support comprehensive health systems strengthening. We found scope for DFID bilateral programmes to do more in this area. This may require innovative approaches to supporting partner governments, for example through providing technical assistance.
Other ODA-funded global health research has yet to be fully aligned with the global health threats agenda, missing opportunities to encourage joined-up medical and social science research, for example on epidemic preparedness and response.
We also found scope for central governance mechanisms to provide greater strategic leadership, for improved communication and coordination between centrally managed global health security programmes and DFID country offices, and for the country offices to play a stronger coordinating role. This would help improve policy and programme synergies across government departments.
Overall, we have awarded a green-amber score for effectiveness. This recognises that the portfolio shows strong potential to be effective. However, there is need for an increased focus on country health systems strengthening and better strategic leadership and coordination of the cross-government portfolio. More could be done to leverage other donor funding and take advantage of relevant ODA-funded research programmes that are currently outside the scope of the Stronger, Smarter, Swifter framework.
Learning: Is learning informing the continuing development of the UK aid response to global health threats?
To answer this question, we have assessed whether the global health threats framework and portfolio have effective mechanisms in place for continued learning, with an emphasis on generating evidence of what works and informing future activity.
In a relatively new policy area, it is important to institutionalise robust evaluation and dissemination mechanisms to help assess and further drive development impact and support value for money. In the case of global health threats policy, the need for coordinated cross-portfolio and cross-country learning is accentuated by the interrelatedness of programming and the cross-border nature of epidemic diseases and drug resistance.
Because the lesson-learning exercise during the Ebola crisis was central to shaping the Stronger, Smarter, Swifter approach, this was dealt with as part of our assessment of the relevance of the strategy. In this section, we assume a more forward-looking perspective, examining whether strong evaluation and lesson-learning processes have been established and made good use of since the adoption of the Stronger, Smarter, Swifter strategy.
Global health security programmes are not yet informed by strong evidence of what works
As yet, there is limited robust evidence on what works in tackling global health threats. Government and external stakeholders interviewed for this review frequently raised questions around what works and how to maximise sustainability, and in particular how much to spend in order to ensure a sufficient level of preparedness.
Consequently, while the global health threats portfolio makes good use of evidence to determine why it is important to intervene, and what areas are in most need of intervention, questions of how to intervene are less well informed by evidence. Specific examples include:
- The case for investing in integrated disease surveillance and response: the business case for Resilient Zero acknowledged that there was no strong evidence available to justify investment in this form of regular electronic surveillance (relative for example to more simple event-based community reporting), despite it having been tested in the field. Although such surveillance systems are recommended by the WHO, we found evidence in Burma, Pakistan and Sierra Leone (concurring with the views of some external experts) that they are expensive to set up and to maintain.
- The Fleming Fund’s business case: similarly, while drawing effectively on the O’Neill review to justify why it should invest in tackling antimicrobial resistance, the business case included less consideration of good practice on developing effective surveillance systems.
The main exception that we found to this weakness was DFID’s Tackling Deadly Diseases in Africa Programme. The business case for this drew heavily on internal learning from previous DFID programmes (Box 14).
Box 14: Learning from the Tackling Deadly Diseases in Africa Programme
DFID’s Tackling Deadly Diseases in Africa Programme was developed in collaboration with the WHO Africa Regional Office. It builds on DFID’s previous £21.5 million programme, UK support for regional preparedness to prevent the spread of Ebola. Between January 2015 and June 2017, this latter programme supported WHO and a civil society network to strengthen disease preparedness and prevent spread across borders in 21 African countries in response to the Ebola outbreak. A range of significant lessons were learnt for optimising interventions and achieving value for money. These lessons strongly informed DFID’s new Tackling Deadly Diseases in Africa Programme, including how to:
- define preparedness and map risks
- measure the impact of prevention activities
- integrate emergency preparedness and response with health systems strengthening
- create and work with civil society networks.
Addressing the evidence gaps will be particularly important for safeguarding value for money, not just in relation to surveillance, but for a whole range of relevant global health security investments. This reinforces the need to capture and share learning from global health threats programmes, to help shape future policy and practice in this field.
Internal lesson-learning is a feature of many global health threats programmes, but formal evaluation processes are highly variable
Some programmes demonstrated strong internal mechanisms for capturing learning and supporting adaptation, through the programme annual review process and more generally. For example, in Sierra Leone, Saving Lives has a significant emphasis on learning and adaptability. There is a planned breakpoint in the middle of the programme, when activities will be updated based on a comprehensive mid-term review conducted by an external monitoring agent, allowing the programme to adapt to changes in the political situation and donor landscape. Recent learning has included the importance of community engagement and behavioural change activities for ongoing health systems strengthening work, leading to changes in how the programme selected partners and activities.
Alongside internal learning and reflection, independently commissioned evaluations are important for providing a more systematic and objective assessment of what works and value for money (including in comparison with external practice). These evaluation reports also help the UK government to demonstrate the effectiveness and impact of investments to other potential donors.
Some global health security programmes have well-developed approaches to evaluation in place. For example, the Fleming Fund has commissioned an external evaluation covering the lifespan of the programme. The Department of Health held supplier engagement events before it commissioned the work, which allowed for early refinement of the evaluation terms of reference. The monitoring agent was then procured alongside the management agent for the Fund, ensuring that the evaluation was more firmly embedded within the delivery of the programme.
However, we found that for the majority of programmes within the portfolio, plans for evaluation are underdeveloped or inadequate. Some programmes have relied on existing internal monitoring procedures to capture lessons learnt, for example the work related to WHO reform, the UK Public Health Rapid Support Team and Resilient Zero in Sierra Leone (despite the wealth of learning to be shared in these areas).
The Department of Health told us that the UK Vaccine Network had plans for an evaluation but this was delayed due to capacity constraints and a focus on commissioning projects. There was evidence of some internal learning informing ongoing programme implementation, but not in a structured or formal way. DFID spoke of the difficulties of assessing research impacts under its Ross Fund research portfolio, and was developing plans to evaluate the outcomes of this work at the time of our review.
We found an even greater weakness in formal plans for disseminating lessons beyond the programmes generating them. In the country programmes we reviewed, we saw evidence of sharing learning with partners locally, but there was little evidence that lessons were being shared more widely, including with other UK government departments. In Sierra Leone, we heard about plans – but no firm commitment – to develop a think piece on the lessons learnt from Resilient Zero and other bilateral programming.
The Fleming Fund and Saving Lives in Sierra Leone are the only programmes we found that set out dissemination plans. The Fleming Fund includes plans for knowledge sharing events, bringing together a wide range of stakeholders, as well as a website to disseminate programme learning.
There is currently no overarching evaluation and learning strategy attached to Stronger, Smarter, Swifter. This means that there is no central guidance on systematic approaches to programme evaluation and learning linked to the global health threats strategy objectives.
DFID and the Department of Health have implemented a range of staff learning activities, but these are not provided consistently across government
As we move further away from the Ebola outbreak, systematic approaches to learning and staff development are required to sustain the knowledge and experience gained during that crisis.
Some positive efforts to share learning on global health security have been made, including through staff development activities. The annual DFID health advisors’ conference, which brings around 70 DFID health advisors together in different locations, is important for sharing knowledge on how to prepare for and respond to global health threats. It has been DFID’s primary mechanism for disseminating internal learning about the Ebola response and related priorities.
In 2016, DFID commissioned a learning resource for health advisors on surveillance, including a reading pack and video presented by Public Health England. Some DFID health advisors also reported considerable learning from country secondments and surge postings to countries such as Sierra Leone during and after the crisis. DFID Sierra Leone now holds a list, updated quarterly, of staff with experience of Sierra Leone or Ebola who could be deployed if required. The office shared this list with DFID’s Democratic Republic of Congo office during their 2017 Ebola outbreak.
Other forums for sharing learning include weekly seminars for DFID health advisors, sometimes including discussions with Public Health England. There are also monthly video conferences with advisors in Asia and Africa to update on policy and technical issues. The Department of Health has introduced a series of internal ODA skills labs in order to increase their knowledge on ODA concepts, tools and processes.
However, existing learning activities are not accessed consistently across the Department of Health and DFID, nor have resources been shared with other ODA-spending government departments and agencies. In our discussions, departmental stakeholders acknowledged that a more comprehensive and shared approach to training, resources and other development for staff working on global health security across government would be valuable.
Outside of DFID’s annual conference, we were told that there is variable engagement from DFID country health advisors in ongoing learning activities. Health advisors in DFID country offices would value a more regular exchange of information on global health threats, both from central government departments and between DFID country offices, including further written resources. Ideas they suggested included:
- the exchange of case studies and good practice examples across DFID country offices, drawn from global health security activities
- a practice aid on DFID’s response to, and lessons and recommendations from, the Ebola outbreak to inform future global health crises
- the opportunity for more discussions with other UK government departments on the global health security agenda
- suitable coordination mechanisms to help facilitate these exchanges, including single points of contact for learning within Whitehall on global health security issues, greater use of DFID’s Health Advisory Network and regional arrangements for sharing learning across DFID country offices.
Strategic-level coordination of evaluation and learning across the portfolio has been weak
During the Ebola outbreak significant emphasis was placed on cross-government learning, in order to diagnose the problems related to epidemic preparedness and response that led to the crisis. While we would not expect efforts to be maintained at this scale, we would expect to see some mechanisms put in place at a strategic level to gather learning on what works. However, we found little evidence of such mechanisms being developed and used to inform programming at the portfolio level.
This is despite a clear need for sharing learning between departments, programmes and DFID country offices, across all themes of Stronger, Smarter, Swifter. We identified opportunities for sharing learning across programmes on issues such as building surveillance systems, partnerships with private sector health care providers and health systems strengthening more broadly (for example between the International Health Regulations Strengthening programme, the Fleming Fund, the Tackling Deadly Diseases in Africa Programme and relevant DFID bilateral programmes).
The need to improve the capture and dissemination of learning from the portfolio of programmes is acknowledged both within government and externally. Some government stakeholders for example noted that it will be important to consider evidence of the emerging effectiveness of the portfolio of programmes targeting global health threats – what has worked well and why – in preparation for the next comprehensive spending review.
We found that the existing high-level governance mechanisms for the global health security portfolio, such as the Global Health Oversight Group, do not adequately encourage the aggregation and exchange of learning. Improvements are needed to secure programme achievements to date and to support the effectiveness and value for money of future efforts to tackle global health threats.
Conclusion on learning
The current global health security portfolio builds on the many lessons from Ebola and related research. However, learning is a continuous process. A variety of UK government and external stakeholders acknowledged the need to improve evaluation and learning mechanisms. We identified some positive examples of learning within individual programmes, as well as some relevant professional development activities, particularly in DFID. However, mechanisms to evaluate programmes and to share programme learning are inconsistent or underdeveloped.
There is significant scope to improve ongoing mechanisms for capturing evidence of what works across the portfolio, for sharing this between government departments, and for ensuring that learning informs the further development of the aid portfolio on global health security. This includes sharing evidence of good practice in accessible formats. Cutting across these challenges, there is currently no overarching evaluation and learning strategy attached to Stronger, Smarter, Swifter to guide learning processes.
We have given the government an amber-red score for its efforts to capture and make use of ongoing learning within its global health threats portfolio. Despite the strong precedent of learning from the Ebola crisis, and some current positive examples, we found that ongoing learning and dissemination is not taking place consistently at the portfolio level and across government departments. Gaps in the mechanisms for capturing institutional learning represent a risk to effectively dealing with outbreaks and epidemics in the future, as well as to value for money.
Conclusions & Recommendations
Conclusions
The UK government has made good progress in developing a coherent framework for addressing global health threats following the Ebola crisis, as well as rapidly establishing a relevant portfolio of programmes and influencing activities. The majority of these activities add value to current donor and other partner activity. The portfolio shows strong potential to be effective, with evidence of positive progress to date, particularly in terms of the WHO and antimicrobial resistance policy influence, supporting a timely response to contain new outbreaks, and building surveillance systems at a country level. New cross-government mechanisms for sharing health threat data and deciding how to respond also show signs of promise.
There is a need to clarify and strengthen the links between global health security and health systems strengthening. Some DFID country health programmes have evolved positively in line with the framework. However, the majority of the global health threats programmes we examined, as well as DFID country strategy documents, could adopt a stronger and more explicit focus on health systems strengthening, including on working closely with national governments. There is also a need to improve coordination between centrally managed global health security programmes and DFID’s country health programmes, including around health systems strengthening objectives.
Other areas for improvement include improving the coordination of ODA-funded global health threats research and marshalling this research to plug gaps in knowledge exposed by the Ebola crisis. The links between the global health threats framework and DFID’s humanitarian policies should be clarified to help improve responses to outbreaks in fragile or conflict-affected settings.
The international environment in which the UK government pursues its global health security agenda is evolving. Coordinating with and influencing other donors, as well as leveraging increased international funding for global health threats, will become increasingly important to avoid duplication of effort and to support the scaling up of activities. There is therefore a need to update the UK’s global health threats strategy and to communicate it more widely.
While some positive learning activities have been introduced, mechanisms to evaluate programmes, and to share cross-portfolio learning consistently across government departments, are underdeveloped. If these are not improved, they could hamper future efforts to respond to global health threats and the value for money of UK aid in this area.
At a strategic level, further efforts are needed to strengthen overall leadership and coordination of the cross-government effort on global health threats in order to help address these challenges and weaknesses.
Recommendations
The following recommendations are intended to help the government, and the Department of Health and DFID in particular, to improve its strategy and interventions, building on the positive momentum achieved since 2015.
Recommendation 1:
The UK government should build on the success of the Stronger, Smarter, Swifter framework by developing a refreshed global health security strategy with a clearer focus on strengthening country health systems, a broader set of research priorities and clearly defined mechanisms for collaboration both across departments and with external actors. The strategy should be published and communicated widely.
Problem statements
- DFID and the Department of Health have not fully articulated the links between global health threats preparedness and health systems strengthening, including the WHO’s building blocks the interface with the International Health Regulations, and the bridging role that bilateral health programmes can play.
- The Stronger, Smarter, Swifter framework is not clear about the roles of other government departments, or wider ODA-funded research programmes, limiting their potential contribution. Broader social science-based research priorities (beyond the research and development of new products) are not articulated within the strategy.
- There is a need to clarify how the range of cross-government coordination mechanisms developed since the Ebola outbreak fit together and support the framework.
- Influencing other actors, including multilateral partners, bilateral donors, philanthropic organisations and the private sector, is critical to the success of the strategy. The growing number of players is threatening the coherence of the international response.
- The Department of Health and DFID have not sufficiently communicated their global health threats framework externally, and coordination mechanisms to engage with other donors and the philanthropic and private sectors (beyond specific programme and project structures) are underdeveloped. This limits the potential for external stakeholders to align their spending and programmes and avoid duplication.
Recommendation 2:
The Department of Health and DFID should strengthen and formalise cross-government partnership and coordination mechanisms for global health threats, broadening their membership where relevant. This should include regular cross-government simulations to rehearse how the UK government might coordinate and respond internationally to a future global health threats crisis similar to Ebola, and engage with other actors such as the WHO.
Problem statements
- Current mechanisms such as the Global Health Oversight Group are overly focused on programme monitoring, leaving important gaps in strategic leadership and coordination – for example to help maximise synergies across the portfolio, leverage other ODA-funded global health research, and drive ongoing learning about what works.
- Programmes funded by the Department of Health currently have governance boards that are formally overseen by the global health security programme board. While this board has some DFID representation, individual DFID programmes do not report to it, further hampering coherence.
- Recommendations from Ebola lesson learning to conduct cross-government simulations or table-top exercises, which would help to ensure that the UK can help deliver an effective and coordinated response to public health emergencies in overseas countries, have not been fully implemented.
Recommendation 3:
The government should ensure that DFID has sufficient capacity in place to coordinate UK global health security programmes and influencing activities in priority countries, including around the objective of strengthening national health systems.
Problem statements
- There is insufficient coordination of global health threats programming in-country to maximise the collective impact of UK programming in areas such as WHO reform, International Health Regulation compliance and health systems strengthening.
- DFID country health advisors have the expertise to fulfil this function. But they are facing increasing capacity challenges as global health threats programming (as well as other bilateral health programmes), and the emphasis on influencing governments and other partners, increases.
Recommendation 4:
DFID and the Department of Health should work together to prioritise learning on global health threats across government, overseeing the development of a broad evaluation and learning framework, regular reviews of what works (and represents good value for money) across global health security programmes, and a shared approach to the training and development of health advisors.
Problem statements
- The supporting evidence base underpinning each programme on what works and cost-effectiveness is generally weak.
- Mechanisms to evaluate individual programmes and to share cross-portfolio learning in a structured way are inconsistent or underdeveloped, which poses a risk to effectiveness and value for money.
- There is currently no overarching evaluation and learning strategy attached to the Stronger, Smarter, Swifter framework, to help drive a consistent and robust approach to evaluation and learning across the portfolio.
- There have been some positive examples of relevant learning exercises carried out to support the professional development of DFID health advisors, but these activities are not shared across government.
Annexes
Annex 1 Detail of scoring
 | Question 1: Relevance Does the UK have a coherent strategy for using aid to address global health threats? |
| The UK government rapidly diagnosed the weaknesses in international systems during the Ebola crisis, and developed a coherent and evidence-based Stronger, Smarter, Swifter strategy for addressing global health threats. The government also established a portfolio of relevant and often pioneering centrally managed programmes and influencing activities, most of which are complementary to other donor activities in this area. There is a need to clarify the links between achieving global health security objectives and strengthening country health systems across the Stronger, Smarter, Swifter framework and within specific programmes. While demonstrating signs of positive evolution since the Ebola crisis, the DFID country health programmes that we examined showed only partial relevance to the framework. The government's strategy should be updated in line with recent external developments. The Stronger, Smarter, Swifter framework should be published and disseminated widely, in order to support the government’s external influencing activities and to help achieve greater synergies with other donors and external actors. |
|
 | Question 2: Effectiveness Is the emerging aid portfolio a potentially effective response to global health threats? |
| The portfolio of global health threats interventions shows strong potential to be effective. There is evidence of positive progress to date, particularly in terms of WHO influence and securing policy commitments to drug resistance, as well as timely and effective responses to contain new outbreaks. The government’s international influencing agenda would benefit from stronger engagement with new actors in the global health threats field, to help leverage donor funding. DFID country programmes are making some positive contributions to epidemic preparedness, but they face tensions in working more closely with governments to support sustainable health systems strengthening. Other ODA-funded research programmes could be better harnessed to support global health security objectives. Cross-government coordination mechanisms could be strengthened to avoid missing important synergies in programming and to help maximise impact. |
|
 | Question 3: Learning Is learning informing the continuing development of the UK aid response to global health threats? |
| The current global health security portfolio builds on the many lessons from Ebola and related research, but since then learning has been weak. We identified some positive examples of individual programme learning and adaptation. However, we found a very mixed commitment to programme evaluation, and that ongoing learning and dissemination is not taking place consistently at the strategy and portfolio levels. Gaps in the mechanisms for capturing institutional learning represent risks to effectively dealing with outbreaks and epidemics in the future. | |
 | Overall score |
| The UK government responded rapidly to address the weaknesses in the international response system exposed by the Ebola crisis, developing a coherent and evidence-based framework for addressing global health threats, and establishing a portfolio of relevant and often pioneering programmes and influencing activities. The portfolio shows strong potential to be effective, particularly in terms of influencing WHO reform, building surveillance systems in high-risk countries, developing new vaccines and supporting a timely response to new outbreaks. Cross-government mechanisms for sharing global health threats data and deciding how to respond also show signs of promise. Building on this strong foundation, there is an opportunity for DFID, the Department of Health and other relevant bodies to do even better. The government’s strategy on global health threats needs to be updated and communicated more widely. The refreshed strategy should emphasise coordination across centrally managed programmes, and with the work of DFID country offices. Country health systems strengthening should feature as a unifying priority across the strategy and programming. The government’s approach to generating and sharing evidence on what works, and mechanisms for transferring knowledge between departments, are weak. Improvements are needed to secure what has been achieved to date and to support the effectiveness and value for money of future efforts to respond to global health threats. |
Annex 2 List of centrally managed global health security programmes and their link to Stronger, Smarter, Swifter
| Programme, budget and lead department | Description | Timescale | |
|---|---|---|---|
| Stronger | Tackling Deadly Diseases in Africa Programme (TDDAP) • Under procurement • DFID | Activities such as strengthening health systems (including the ability and accountability of African country health systems to achieve compliance with the International Health Regulations), assessing data, and table-top exercises to stop deadly diseases in Africa getting out of control and reaching the UK and other countries. | July 2017 – March 2020 |
| Tackling drug-resistant malaria • £8.4m • DFID | Supporting the Asia Development Bank's programme to contain the spread of drug-resistant malaria in South East Asia, in combination with governments in the region and development partners. | Nov 2013 – June 2018 | |
| UK support for regional preparedness to prevent the spread of Ebola • £21.5m • DFID | Forerunner of TDDAP outlined above. Included activity designed to support communities in countries at risk to be better equipped to prevent the spread of Ebola and similarly communicable diseases as well as helping to strengthen national health systems. | 2015 – 2017 | |
| Core Voluntary Contribution (CVC) to World Health Organization (WHO) • £58m • DFID | Funding to support WHO reforms including the organisation’s approach to risk and financial management; transparency; value for money; budget allocations to key priorities; partnership working and providing effective leadership. | Dec 2016 – March 2020 | |
| International Health Regulations (IHR) Strengthening Programme • £16m • Department of Health | Department of Health commissioned Public Health England (PHE) to promote compliance with the IHRs, by helping to strengthen public health systems and technical capabilities in (6) ODA-eligible lower and middle income countries, in global agencies, and in the regional institutions/mechanisms responsible for supporting implementation. | Nov 2016 – March 2021 | |
| Total budget for centrally managed global health threats programmes falling under the ‘Stronger’ category: £103.9m (17% of total funding) (excluding GAVI) DFID: £87.9m (85% of ‘stronger’ funding) Department of Health: £16m (15% of ‘stronger’ funding) |
|||
| Smarter | Ross Fund • overall budget £1bn, including the UK Public Health Rapid Support Team | The Ross Fund is a portfolio of interventions, some of which fall within the global health security area with others aimed at supporting more longstanding health challenges. | 2016/17 – 2021/22 |
| Fleming Fund • £265m • Department of Health | The Fleming Fund is intended to support low and middle-income countries to tackle antimicrobial resistance (AMR) through supporting the development of laboratory capacity, surveillance systems and the use of data to identify resistance. | April 2016 – March 2021 | |
| UK Vaccine Network • £110m • Department of Health | The UK Vaccines Network aims to identify and support the initial development of a set of priority vaccines and vaccine technologies to help tackle diseases with epidemic potential. | April 2016 – March 2021 | |
| WHO Blueprint • £6m • DFID | Funding to support the WHO Blueprint, a global strategy and preparedness plan to facilitate rapid research during epidemics, fast-tracking tests, vaccines and medicines that can be used to save lives and avert large-scale crises. | 2017/18 – 2021/22 | |
| DFID Wellcome Trust • £19m • DFID | Development of a flexible funding mechanism to support priority research in response to disease outbreaks and fund research into more effective preparedness and response activities. | 2016 – 2021 | |
| FIND • £30m • DFID | Support for the Foundation for Innovative New Diagnostics (FIND) to develop easy to use diagnostics for diseases where there is currently limited research and development investment. | 2017/18 – 2021/22 | |
| AMR Innovation Fund • £50m • Department of Health | Funding to help develop international partnerships to support research and development to tackle AMR, focused on neglected /underfunded areas of AMR research and leveraging additional financing from other countries and non-state actors. | April 2016 – March 2021 | |
| Biopreparedness Organisation • £16m • Department of Health | Investing in bio-preparedness to further work on development of infectious disease vaccines and drugs. | April 2016 – March 2021 | |
| Access to Medicines Index and Antimicrobial Resistance Index • £4.9m • DFID | Financial support to the Access to Medicine Foundation to deliver two further versions (2018, 2020) of the Access to Medicines Index, ranking the efforts of pharmaceutical companies on how they make medicines, vaccines and diagnostics more accessible, and a new Anti-Microbial Resistance Index. | Sept 2016 – March 2021 | |
| Total budget for centrally managed global health threats programmes falling under the ‘Smarter’ category: £500.9m (79% of total funding) DFID: £59.9m (12% of ‘smarter’ funding) Department of Health: £441m (88% of ‘smarter’ funding) |
|||
| Swifter | UK Public Health Rapid Support Team (RST) • £20m • Department of Health | The RST is a team of public health experts on permanent standby that can rapidly respond to invitations to investigate, respond and research a possible or known disease outbreak. The project is being undertaken by a partnership of PHE (£10m) and the London School of Hygiene and Tropical Medicine (£10m). | April 2016 – March 2021 |
| WHO Contingency Fund for Emergencies (CFE) • £6.2m • DFID | Contribution to a WHO emergency fund intended to fill a critical gap from the beginning of a health emergency until resources from other financing mechanisms begin to flow.. | Dec 2015 – Feb 2017 | |
| UK investment in Gavi, the Vaccine Alliance • £1.5bn (core funding) • DFID | Funding for Gavi, an international organisation created in 2000 to improve access to new and underused vaccines for children living in the world’s poorest countries. * Note: Gavi is an existing programme with small focus on global health threats relative to non-epidemic disease. | 2016 – 2020 | |
| Total budget for centrally managed global health threats programmes falling under the ‘Swifter’ category: £26.2m (4% of total funding) DFID: £6.2m (24% of ‘swifter’ funding) DH: £20m (76% of ‘swifter’ funding) |
|||
| Total budget for all stronger, smarter, swifter programmes on global health threats: £631m (excluding GAVI) DFID: £154m (24% of overall funding) Department of Health: £477m (76% of overall funding |
|||
Annex 3 ODA-funded research programmes of relevance to global health threats
| Fund | Description | Example projects/research units |
|---|---|---|
| Global Challenges Research Fund (Department for Business, Energy and Industrial Strategy, £1.5bn, 2016-21) | Supports research aimed at tackling global challenges, by addressing the problems faced by developing countries in the UK’s national interest. Health topics have included an ‘Infectious Disease research’ call as well as a £4m ‘Zika research’ call. | Building resilient health systems: lessons from international, national and local emergency responses to the Ebola epidemic in Sierra Leone, the London school of Hygiene and Tropical Medicine, £502,785. Community health volunteers as mediators of accessible and responsive community health systems: lessons from the Health Development Army in Ethiopia, the London school of Hygiene and Tropical Medicine, £106,622. Zika: Estimating the transmission and case burden of Zika virus in Kenya, University of Oxford, £149,996. Zika: Development of a type specific Zika virus antibody assay for use in Brazil, University College London, £121,935. |
| Newton Fund (Department for Business, Energy and Industrial Strategy, £735m, 2014-2021) | Builds research and innovation with partner countries to support economic development and welfare, through collaboration and match funding. It includes a cross-council antimicrobial resistance (AMR) initiative with India (£7.5m). | Funded research includes neglected diseases in Brazil, Thailand and Vietnam, AMR in South Africa, and Health systems strengthening in Brazil. |
| Antimicrobial Resistance Cross-Council Initiative (UK Medical Research Council and Economic and Social Research Council lead with Department of Health, £9m, 4 years) | There are two cross-council initiatives: Drivers of AMR in low and middle income countries and AMR: Behaviour within and beyond the healthcare setting. | Spatial and temporal dynamics of AMR transmission from the outdoor environment to humans in urban and rural Bangladesh, Loughborough University. Infection prevention and control for drugresistant tuberculosis in South Africa in the era of decentralised care: a whole systems approach, London School of Hygiene and Tropical Medicine |
| National Institute for Health Research (NIHR) Global Health Research Programme (Department of Health, £429.5m, 2016-2021) | Supports applied global health research for the direct and primary benefit of patients and the public in low and middle-income countries. Funding is not ring-fenced for particular topics. | NIHR Global Health Research Unit on Tackling Infections to Benefit Africa, The University of Edinburgh, £6.9m. NIHR Global Health Research Unit on Genomic Surveillance of Antimicrobial Resistance, Wellcome Trust Sanger Institute, £6.9m. NIHR Global Health Research Unit on Health Systems Strengthening in Sub-Saharan Africa, King's College London, £7m. |
| Joint Global Health Trials Initiative (UK Medical Research Council, DFID, Wellcome Trust, Department of Health via NIHR, £220m, 2011-2027) | Supports clinical trials researching interventions into the major causes or morbidity and mortality in middle and low income countries. | In 2016, alongside funding many projects on malaria, one on HIV and one on meningitis, two projects were funded to develop the Ebola vaccine. |
| Research for Health in Humanitarian Crises (DFID and Wellcome Trust, £2m each call, 2016-2021) | Supports collaborative research on public health challenges in humanitarian crises. Includes three categories relevant to global health threats: Ebola research; research relating to health systems and resilience; and communicable diseases, surveillance and modelling. | Systems resilience in UNRWA health provision to Palestine refugees displaced by Syria crisis, Queen Margaret University, Edinburgh, £335,203. Social marketing strategy promoting Ebola treatment-seeking behaviour, Umea University, Sweden, £158,547. Participatory behavioural change to reinforce infection prevention, International Rescue Committee, £185,621. |
| Resilient and Responsive Health Systems (RESYST) (DFID, £8m, 2010-18) | International research consortium focusing on health policy and systems research in Africa and Asia. The three funding categories are financing, health workforce and governance. | Investing in private nurse training institutes and their role in addressing human resources constraints, African Medical and Research Foundation. Guidelines for accountability in the implementation of the primary health care fund, University of Nigeria |
Annex 4 UK bilateral contributions to health systems strengthening
Evidence of UK bilateral contributions to country health systems strengthening among programmes examined by the review
- Health services – in Burma, the 3MDG Fund’s focus on expanding access to health care services in ethnic minority and conflict areas (including through the development of partnerships with ethnic community organisations) has resulted in increased tuberculosis case detection and prevention of multi-drug-resistant tuberculosis. Future plans include establishing specialist treatment facilities in the Yangon and Mandalay regions. In Nigeria, the £133 million Maternal and Newborn Child Health 2 (MNCH2) programme scored particularly well in its latest annual review on support for primary health care facilities.
- Health workforce – in Sierra Leone, DFID commissioned a health worker census and payroll verification exercise through Saving Lives, and is now providing support for the development of a National Human Resources for Health strategy, as well as training for health workers. In Burma, through the 3MDG Fund, DFID supported the ministry in strengthening the midwifery workforce, including their pre-service education and the national regulation for their training.
- Health information systems – in Burma, the 3MDG Fund supports the ministry in implementing the Health Management Information System module of the District Health Information System, an electronic platform to manage, aggregate and analyse data collected at health facilities in 49 townships across the country. In Sierra Leone, in addition to improving disease surveillance and response, Resilient Zero has enhanced the capacity of district health management teams to interpret and use routine health data. In Pakistan, Public Health England has completed the situation and political economy analysis to support the revitalisation of the surveillance system.
- Access to essential medicines – in Burma, programme work (£12 million) to tackle drug-resistant malaria was successful in expanding the availability of quality assured drugs in private sector outlets through reducing their relative price in most areas. In Nigeria, MNCH2 has established logistics working groups, reviewed existing drug guidelines and supported the quantification of medical equipment and drugs.
- Financing – the MNCH2 programme in Nigeria has helped states access federal grants under a World Bank payment by results programme. Across a number of countries, UK advocacy for an increased share of state revenues to be spent on health was recognised as an ongoing priority, especially for countries transitioning from recent crises.
- Leadership/governance – UK programmes in Sierra Leone and Burma have contributed to the establishment of national health sector plans, which are now guiding further programme investments in health systems strengthening. In Nigeria, DFID has also assisted the Federal Ministry of Health in health sector policy formation.